Abstract
Aims
To report risk factors for visual acuity (VA) improvement and harm following cataract surgery using electronically collected multi-centre data conforming to the Cataract National Dataset (CND).
Methods
Routinely collected anonymised data were remotely extracted from the electronic patient record systems of 12 participating NHS Trusts undertaking cataract surgery. Following data checks and cleaning, analyses were performed to identify risk indicators for: (1) a good acuity outcome (VA 6/12 or better), (2) the pre- to postoperative change in VA, and (3) VA loss (doubling or worse of the visual angle).
Results
In all, 406 surgeons from 12 NHS Trusts submitted data on 55 567 cataract operations. Preoperative VA was known for 55 528 (99.9%) and postoperative VA outcome for 40 758 (73.3%) operations. Important adverse preoperative risk indicators found in at least 2 of the 3 analyses included older age (3), short axial length (3), any ocular comorbidity (3), age-related macular degeneration (2), diabetic retinopathy (3), amblyopia (2), corneal pathology (2), previous vitrectomy (2), and posterior capsule rupture (PCR) during surgery (3). PCR was the only potentially modifiable adverse risk indicator and was powerfully associated with VA loss (OR=5.74).
Conclusion
Routinely collected electronic data conforming to the CND provide sufficient detail for identification and quantification of preoperative risk indicators for VA outcomes of cataract surgery. The majority of risk indicators are intrinsic to the patient or their eye, with a notable exception being PCR during surgery.
Similar content being viewed by others
Introduction
Monocular visual acuity (VA) is widely used as an outcome measure following cataract surgery despite its known limitations.1 The near universality of its use and the relative ease with which it can be collected mean that this practice is likely to continue in the foreseeable future, at least until a validated and well-accepted alternative is developed. Routine collection of clinical data using electronic patient records has made it possible to undertake multi-centre audit and analysis of significant numbers of cataract surgical procedures through extraction and aggregation of detailed and standardised clinical records data. In the current report from our collaborative series,2, 3, 4, 5, 6, 7, 8 we provide information on risk indicators for VA outcomes of cataract surgical procedures.
Materials and methods
The method of extraction and aggregation of multi-centre data has previously been reported.6 Extracted data included pre-, intra-, and postoperative data.
VA data were recorded in one or more of three ways at each clinical encounter. These were uncorrected, corrected (habitual or best correction), and using a ‘pinhole’ correction. As before, we have pragmatically designated the term ‘best-measured VA’ preoperatively as the better VA either corrected (habitual/best correction) or uncorrected (UCVA); where no result was available for either of these two measures, pinhole VA was resorted to as a proxy. In contrast, postoperatively the ‘best-measured VA’ was the best VA obtained from any one of: the corrected VA (usually best-corrected VA (BCVA), ie, optimal postoperative refraction), the UCVA, or the pinhole VA.6 In some contributing centres postoperative VA data were collected before postoperative refraction, which necessitated the inclusion of pinhole correction on such occasions.
Three multivariable risk factor analyses were undertaken with the STATA statistical software package to examine different aspects of monocular VA outcomes. Logistic regression was used to assess candidate indicators for a good VA outcome (6/12 or better), multiple regressions for pre- to postoperative change in VA, and logistic regression for the analysis of risk indicators for clinically significant visual loss following surgery (doubling or worse of visual angle pre- to postoperatively). Snellen acuities were converted to LogMAR acuity for analyses; all analyses included adjustment for preoperative baseline VA (as a continuous variable) and adjustment for paired eyes to acknowledge within-patient inter-eye correlation. The following terms were included in each model: age, sex, any ocular comorbidity, age-related macular degeneration, glaucoma, diabetic retinopathy, brunescent/white cataract, high myopia, corneal pathology, amblyopia, uveitis/synechiae, no fundal view/vitreous opacities, pseudoexfoliation/phacodonesis, previous vitrectomy, previous retinal detachment surgery, axial length (quintiles), pupil size, inability to co-operate, unable to lie flat, any alpha blocker, tamsulosin, doxazosin, alfuzosin, indoramin, prazosin, terrazosin, surgeon grade, and posterior capsule rupture (PCR) during surgery. Stepwise forward and backward fitting was used for each of the models, which were restricted to main effects as the number of potential interaction terms would have been unmanageable. The final models were assessed for fit using the C-Stat or area under the receiver–operator characteristics curve for logistic regressions and R2 for multiple regression.
Results
In all, 406 surgeons from 12 NHS Trusts submitted data on 55 567 cataract operations between November 2001 and July 2006 (86% from January 2004). Preoperative ‘best-measured’ VA was known for 55 528 (99.9%) and postoperative ‘best-measured’ VA outcome for 40 758 (73.3%) operations (median follow-up 35 days). Optimal postoperative refracted VA or BCVA was available for 24 404 eyes (43.9%).
Good outcome: VA 6/12 or better
Postoperatively 37 096 (91.0%) eyes achieved 6/12 or better acuity. The results of the logistic regression for factors significant at the 5% level, adjusted for baseline VA, are presented in Table 1. Because of a large sample size and a relatively common outcome (91.0%) the statistical power of this model was high and for this reason caution should be exercised when interpreting small effects with limited statistical significance such as 0.67<OR<1.5 and/or 0.05<P<0.01 as these may be clinically unimportant. Table 1 shows that factors with OR<1 were less likely and those with OR>1 were more likely to be associated with a good VA outcome of 6/12 or better. Factors with OR>1.5 associated with a good VA outcome included: brunescent/white cataract and no fundal view/vitreous opacities. Similarly, factors with OR<0.67 associated with a less favourable VA outcome (worse than 6/12) included: older age, short axial length, any ocular comorbidity, age-related macular degeneration, diabetic retinopathy, amblyopia, corneal pathology, previous vitrectomy, the alpha blocker prazosin, and PCR during surgery.
Change in VA pre- to postoperatively
The results of the multiple regression analysis for change in VA from pre- to postoperative status are presented in Table 2, adjusted for baseline VA. The effect sizes (ESs) are formatted as LogMAR lines (five letters per line, eg, one line change equivalent Snellen 6/12 to 6/9+ or 6/30 to 6/24). The average change between preoperative VA (0.54 LogMAR, equivalent Snellen 6/21 approximate) and postoperative VA (0.14 LogMAR, equivalent Snellen 6/8 approximate) was 4.0 LogMAR lines or 20 LogMAR letters improvement. Factors with +ve values represent associations with greater than average improvement and factors with −ve values represent associations with worse than average improvement. This model was likewise highly statistically powered and again caution should be exercised in interpretation of small ES such as less than half a LogMAR line above or below average, that is, ≤±2 LogMAR letters or 0.4 LogMAR lines difference (equivalent Snellen 6/12 to 6/13 approximate) and/or borderline statistical significance 0.05<P<0.01 as these may be clinically unimportant. Based on these criteria it can be seen from Table 2 that the only factor with a non-trivial ES (>+0.4 LogMAR lines) associated with better than average VA improvement was brunescent/white cataract, and the magnitude of this effect was only slightly more than half a line better than the average improvement. On the other hand there were many factors that were associated with more than two letters below average improvement (ES<−0.4 LogMAR lines): older age, short axial length, any ocular comorbidity, age-related macular degeneration, diabetic retinopathy, amblyopia, corneal pathology, previous vitrectomy, previous retinal detachment surgery, and PCR during surgery.
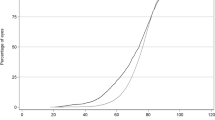
VA loss of ≥3 LogMAR lines of acuity
Clinically significant vision loss was defined as a doubling or worse of the visual angle (loss of 3 LogMAR lines) between pre- and postoperative assessments (eg, LogMAR 0.3 to 0.6 or equivalent Snellen 6/12 to 6/24). There were 507 (1.24%) eyes that experienced this level of loss of vision. The risk indicators for acuity loss are presented in Table 3, adjusted for baseline VA. In this table an OR<1 indicates that the factor is protective against loss of vision and an OR>1 indicates that the factor is associated with a higher risk of VA loss. Because the outcome of interest was relatively uncommon (1.24%) statistical power was less and there is less justification for a strict interpretation of small effects as clinically unimportant though the use of multiple testing should be borne in mind where 0.05<P<0.01. Significant factors associated with loss of vision were older age, short axial length, any ocular comorbidity, diabetic retinopathy, small pupil size, and PCR during surgery, the latter being the most powerful factor with an OR of 5.74.
Discussion
In these analyses of a large sample of routine NHS cataract operations we have focused on three related but slightly different aspects of postoperative monocular VA outcome: good VA (LogMAR ≤0.3, ie, Snellen 6/12 or better), change in VA pre- to postoperatively, and loss of VA with doubling or worse of the visual angle pre- to postoperatively. This approach has allowed different aspects of outcome to be highlighted separately with good VA outcome indicators for a favourable end result, change in VA probing indicators for the effectiveness of surgery to improve VA, and loss of VA probing indicators for acuity loss related to surgery. Not surprisingly, several of the significant risk factors found were common to all three analyses, though certain interesting differences also emerged.
In overview, the results appeared favourable, with analyses indicating substantial levels of VA benefit and low levels of harm. Thus, 91% of the eyes achieved a favourable outcome of 6/12 or better with an average VA improvement of 4.0 LogMAR lines (20 LogMAR letters; equivalent Snellen 6/21 to 6/8 approximate). A clinically significant loss of vision with doubling of the visual angle occurred in 1.24% of eyes, indicating that surgery was relatively safe, with perioperative damage to vision being reasonably uncommon.
The important adverse preoperative risk indicators found in at least two of the three analyses included older age (3), short axial length (3), any ocular comorbidity (3), age-related macular degeneration (2), diabetic retinopathy (3), amblyopia (2), corneal pathology (2), previous vitrectomy (2), and PCR during surgery (3). All these preoperative adverse risk indicators are outside of the surgeon's control. Appropriate actions, however, would include ensuring that the patient is correctly informed of a guarded prognosis, and, where surgical difficulty is anticipated (eg, corneal pathology or previous vitrectomy), that the operation is undertaken by a suitably experienced surgeon. When interpreting our results it should be born in mind that all the specific comorbidities listed were also included within the ‘Any Ocular Comorbidity’ category. Within the statistical models a small proportion of the effect from the itemised comorbidities may have contributed to the ES of ‘Any Ocular Comorbidity’, but there were also a range of less common comorbidities, included in ‘Other’, which individually were not important but when grouped together formed a significant group.
PCR deserves special consideration and this complication has long been regarded as a benchmark for the quality of cataract surgery. In all three of our analyses, this operative event was found to be highly statistically significant. Associated with this event was a 59% reduction (OR=0.41) in the likelihood of achieving a good outcome (6/12 or better); eyes on average had 1.12 LogMAR or just over one line (5.6 LogMAR letters) less improvement in vision, and there was a 5.74 times increased likelihood of eyes with PCR suffering loss of vision to the extent of a doubling or worse of the visual angle. These results underline the importance of avoiding PCR whenever possible by adopting strategies to minimise this risk for patients whose predicted probability of a capsule rupture is elevated. Our previous work has drawn attention to the preoperative factors associated with capsule rupture and the importance of ensuring that appropriately skilled surgeons undertake higher-risk operations.2, 5 The most experienced and highly skilled surgeons are not only best placed to anticipate and head off intraoperative difficulties as surgical events unfold, but in the event of a complication they are also best placed to deal with an adverse surgical situation in a way that minimises, as far as possible, resulting harm.
Unexpectedly, ‘brunescent or white cataract’, and less consistently ‘no fundal view/vitreous opacities’, appeared to be associated with enhanced VA benefit from surgery. In the absence of other explanations it is possible that this observation may have arisen as a result of inaccurate adjustment for baseline acuity. Many of these eyes are likely to have had very poor preoperative VA and at the extreme end of the scale our method of LogMAR VA extrapolation may well have been inaccurate and produced a spurious result (ie, CF, HM, and PL scored as LogMAR 2.1, 2.4, and 2.7, respectively). Alternatively, these cases may have been handled by the most highly skilled surgeons who were able to make the most of a difficult surgical challenge. However, the first logistic regression model included surgical grade, so this effect was accounted for in the analysis as presented, and in the other two models the effect of surgical grade was not found to be statistically significant.
Our findings are in keeping with a number of earlier studies. It is to be expected that poor preoperative VA would be associated with large improvements in VA following uneventful surgery; a ceiling effect on the VA scale means that there is less ‘room for improvement’ for eyes with relatively good preoperative VA. Each of our analyses was adjusted for preoperative VA to account for this expectation. Older age, ocular comorbidity and ‘surgical complexity’ have also previously been noted as being associated with a worse VA outcome.9, 10, 11, 12
One of the strengths of our study is the large sample size and the wealth of detailed preoperative data available for analysis. This can only be achieved through prospective routine electronic data collection, the analysis being a by-product of routine clinical care. This approach has allowed us to uncover a number of previously unidentified specific risk indicators for adverse monocular VA outcome following cataract surgery. In our sample the completeness of the preoperative data was very high,5, 6 but because of varying patterns of patient care in different centres we did not have the same levels of data completeness for postoperative VA outcome (73.3%), which we acknowledge as a relative weakness.
Conclusion
Our objective with this analysis was to examine predictors of monocular VA outcome from a number of different perspectives. In keeping with earlier studies, we have confirmed that older age, ocular comorbidity, and operative complications are associated with worse outcomes. To this we have added detailed information regarding the risks for specific types of ocular comorbidity. An important finding is the magnitude of the impact of capsule rupture on VA outcome, in particular its strong association with VA loss (OR=5.74; <0.0001). This powerful finding underlines the relevance and importance of PCR as an accepted benchmark of surgical quality.
As an outcome, monocular VA does, however, have significant limitations, as it does not fully reflect the overall visual experience of the person who has undergone surgery. Patient-reported outcome measures will in future be needed to address postoperative outcome more fully.

References
Lotfipour S, Patel BH, Grotsky TA, Anderson CL, Carr EM, Ahmed SS et al. Comparison of the visual function index to the Snellen visual acuity test in predicting older adult self-restricted driving. Traffic Inj Prev 2010; 11: 503–507.
Sparrow JM, Taylor H, Qureshi K, Smith R, Johnston RL, UK EPR user group. The cataract national data set electronic multi-centre audit of 55,567 operations: case-mix adjusted surgeon's outcomes for posterior capsule rupture. Eye (Lond) 2011; 25: 1010–1015.
Knox Cartwright NE, Johnston RL, Jaycock PD, Tole DM, Sparrow JM . The Cataract National Dataset electronic multicentre audit of 55,567 operations: when should IOLMaster biometric measurements be rechecked? Eye (Lond) 2010; 24: 894–900.
Johnston RL, Taylor H, Smith R, Sparrow JM . The Cataract National Dataset electronic multi-centre audit of 55,567 operations: variation in posterior capsule rupture rates between surgeons. Eye (Lond) 2010; 24: 888–893.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye 2009; 23: 31–37.
Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Galloway P et al. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye 2009; 23: 38–49.
El-Hindy N, Johnston RL, Jaycock P, Eke T, Braga AJ, Tole DM et al. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: anaesthetic techniques and complications. Eye 2009; 23: 50–55.
Benzimra JD, Johnston RL, Jaycock P, Galloway PH, Lambert G, Chung AK et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: antiplatelet and anticoagulant medications. Eye 2009; 23: 10–16.
Perea-Milla E, Vidal S, Briones E, Aguirre U, Baré M, Fernández de Larrea N et al. Development and validation of clinical scores for visual outcomes after cataract surgery. Ophthalmology 2011; 118: 9–16.
Saw SM, Tseng P, Chan WK, Ong SG, Tan D . Visual function and outcomes after cataract surgery in a Singapore population. J Cataract Refract Surg 2002; 28: 445–453.
Norregaard JC, Hindsberger C, Alonso J, Bellan L, Bernth-Petersen P, Black C et al. Visual outcomes of cataract surgery in the United States, Canada, Denmark, and Spain. Report from the International Cataract Surgery Outcomes Study. Arch Ophthalmol 1998; 116: 1095–1100.
Schein OD, Steinberg EP, Cassard SD, Tielsch JM, Javitt JC, Sommer A . Predictors of outcome in patients who underwent cataract surgery. Ophthalmology 1995; 102: 817–823.
Acknowledgements
This work was supported by a grant from the Academy of Medical Royal Colleges entitled ‘Developing a defensible decision making algorithm for revalidation based on case mix adjusted measures of surgical performance’, which was administered through the Royal College of Ophthalmologists.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
RL Johnston is a Director of Medisoft Limited. The other authors declare no conflict of interest.
Additional information
Sections of this work have been presented at the Bristol Eye Hospital Bicentennial Celebration, June 2010 and the Academy of Medical Royal Colleges, December 2010.
Rights and permissions
About this article
Cite this article
Sparrow, J., Taylor, H., Qureshi, K. et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: risk indicators for monocular visual acuity outcomes. Eye 26, 821–826 (2012). https://doi.org/10.1038/eye.2012.51
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.51
Keywords
This article is cited by
-
Visual function loss in fungal sphenoid sinusitis: clinical characteristics and outcomes
Scientific Reports (2024)
-
A model for anterior vitrectomy in real patients: Simulation for practical training
Eye (2024)
-
How old is too old for routine cataract surgery?
Eye (2023)
-
The effect of ethnicity on anatomic success following macular hole surgery: a multicentre cohort study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Combined phacoemulsification surgery and intravitreal triamcinolone injection versus stand-alone surgery in patients with type 2 diabetes: a prospective randomized trial
BMC Ophthalmology (2022)