Abstract
Purpose To assess the patients who have had photodynamic therapy (PDT) in the Northern region of the UK, in relation to the eligibility criteria found to benefit in the TAP study (treatment of age-related macular degeneration with photodynamic therapy study), so as to make an estimate of the number of patients who might benefit from this treatment and to present the outcome of the treatment so far.
Method The records and fluorescein angiograms (FFAs) of all patients who had had PDT in the Northern region between 2001 and 2002 were reviewed for compliance with the TAP criteria of >50% classic choroidal neovascularization and >34 letters on the 2 m logMAR Early Treatment Diabetic Retinopathy Study chart. NHS funding has been available in the Northern Region since January 2001 for ‘second eye’ involvement. A review of all the angiograms performed for exudative macular degeneration in 1 year was also performed. The visual outcome of those patients 1 year from baseline was measured.
Results A total of 82 ‘second eye’ patients were treated between January 2001 and December 2002. This gives an incidence of 65 per 3 million and so about 1300 in the whole of the UK (population 60 million). In all, 238 FFAs were performed on exudative macular degeneration, with 21% being found eligible for PDT. As of February 2003, 54 TAP criteria, macular degeneration patients were 1 year from initial treatment. Of these, 12 had incomplete follow-up and 13 patients had lost more than 15 letters. The responder rate defined as losing <15 letters was 42−13/42=69%. Seven of those who did not make 1-year follow-up had lost more than 15 letters when last seen, giving a responder rate of 54−20/54=63%.
Conclusion There may not be as many patients eligible for PDT, using the TAP criteria, as previously hoped. The outcome of treatment appears similar to that found in the TAP study.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the most common cause of blindness in the above 50 age group in the developed world. By 2020, it has been estimated that up to 7.5 million, of the over 65 population, may suffer from vision loss due to AMD.1
Photodynamic therapy (PDT) has been shown to reduce the risk of moderate and severe visual loss at 1- and 2-year follow-up in the TAP study, in a subgroup of patients; those with subfoveal, predominantly classic, choroidal neovascular membranes (CNV) and initial vision of 6/60 or better (34 letters on the 2 m EDTRS chart).2,3,4 There are no data available for the incidence of such treatable patients arising in a particular population. Such information would be helpful in planning service provision for PDT and for further possible treatments being developed for CNV.
National Health Service (NHS) funding for PDT has been available in the Northern Region since January 2001 for the second eye, that is, the first eye already having poor vision from any cause. This was in keeping with the National Institute of Clinical Excellence (NICE) guidance, although this may alter in the future. Therefore, no ‘second eye’ patients were excluded due to lack of funds.
Patients were deemed eligible for treatment if they satisfied the criteria found to benefit from PDT in the TAP study. All patients in the Northern Region were referred to one treatment centre, The Royal Victoria Infirmary, Newcastle (RVI), over this time period, and there was little private provision of this treatment outside the treating centre. (In all, 10 patients were treated in the only other centre offering private PDT in the 2 years. Two were for ‘first eyes’, one for ‘second eye’, three for occult and four unknown (personal communication). The FFAs have not been reviewed.) Therefore, we are able to provide figures for the incidence of patients in a defined population, who were eligible for and actually received ‘second eye’ PDT under our present referral systems, for the 2 years 2001 and 2002.
To try and put this figure in the context of the total number of patients with exudative AMD, an analysis of all fluorescein angiograms (FFAs), performed in 2002 at the RVI, for a provisional diagnosis of exudative AMD, is presented. The figures for non-AMD cases of classic CNV are also included so as to compare the frequency; however, funding was variably available for these patients.
The outcome of patients in terms of compliance with 3-month follow-up, number of treatments, change in visual acuity and adverse events are presented for those at 1 year from initial treatment.
Methods
The number of patients eligible and actually treated with PDT in the Northern Region in the years 2001 and 2002 were calculated. NHS funding for PDT has been available in the Northern Region since January 2001 for the ‘Second’ eye, that is, the ‘first eye’ already having poor vision, ≤6/36, from any cause. Patients were deemed eligible for treatment if they were likely to benefit, as defined by the TAP study, that is, those with subfoveal predominantly classic (CNV) and initial vision of ≥34 letters on the 2 m Early Treatment Diabetic Retinopathy Study (EDTRS) charts logMAR chart (equivalent to 6/60 or better).2,3,4 Patients with a classic membrane, as a recurrence from focal argon laser, were also included. Myopic patients with a more than minus 6 D correction were not included in this study. The RVI was the only provider of PDT treatment for seven Health Authorities. The population figures for those over 65 were known.
Patients thought to be eligible for PDT were referred for consideration for the treatment from their ophthalmologist. FFA and visual acuity data were provided and a decision made by one of us (SJT) on likely eligibility, based on the TAP criteria outlined above. Treatment was allowed on a named patient basis by the funding authorities. If a patient was thought eligible permission was sort, the patient sent information to allow informed consent and an appointment made, on average, 2 weeks later. At the clinic visit the following were carried out and recorded: refracted 2 m logMAR visual acuity, using the TAP protocol;2 digital stereo FFA; lesion size measurement; clinical examination.
The TAP visual acuity scoring system involves recording the total number of letters seen at 2 m plus 15 (assumes that they will read the top three lines at 1 m). If the patient reads fewer than 20 letters at 2 m, the patient is tested on the top three lines at 1 m and the total letter score was the total number of letters read at 2 m plus the letters read at 1 m.
If the patient was deemed eligible and consented for treatment, this was then performed using the same needle, which was still in situ from the FFA. The patients were then seen at 3-monthly intervals for possible retreatment. At 1 year, a refracted 2 m logMAR visual acuity was again recorded. The FFA and visual acuity data have further been retrospectively reviewed by one of us (SJT) to check compliance with the TAP criteria.
All the FFAs for 2002 at the RVI performed for exudative AMD, either looking for CNV or to confirm a diagnosis, were analysed by both (SJT and LC). Prospective information on provisional diagnosis and Snellen visual acuity had been documented on all FFAs in 2002 and stereo FFAs taken for all cases of AMD. ‘First’ or ‘second’ eye involvement was recorded. If both eyes had active disease, this was grouped with ‘second’ eyes and FFA data recorded from the eye with better vision. If more than one FFA had been recorded on a patient in the year, only the initial one was used. The FFAs of patients treated with PDT from the catchment area of the RVI were included to allow a calculation of the incidence of treatable cases in patients seen with exudative AMD. FFAs on patients from outside the area were excluded. The visual acuity data were collected for the eye with active disease. If both eyes were involved, visual acuity from the better eye was recorded.
The MPS Group terminology was used for the FFA classification.5 The FFAs in those patients who had PDT were classified into 100% classic and >50% classic. The classic CNV was defined as early hyperfluorescence, maybe with a lacy edge, that increased in intensity and spread beyond its initial borders, that is, leaked. In 100% classic lesions, this is often associated with a dark halo and surrounding blush. The other components recorded were: blood if >10%; serous pigment epithelial detachment (PED) (sharply defined pooling of fluorescein); elevated blocked fluorescence (often found in the centre of larger CNV); elevated staining (associated with fibrosis); occult CNV type 1, fibrovascular PED (elevated retinal pigment with a stippled appearance on FFA); type 2 (late leak of undetermined origin).
The FFAs for all cases with a provisional diagnosis of exudative AMD, but which were not treated with PDT, were classified into the following groups: >50% classic; <50% classic; occult type 2 (late leak) <4 disc areas; mixed occult (blood, PEDs, blocked fluorescence); type 1 occult (fibrovascular PED) only, serous PED only; dry and other diagnosis. Peripapillary CNV were not included.
Results
The incidence of patients, fitting the ‘TAP’ criteria, who underwent PDT in their ‘second’ eye over the period 2001–2002 is presented (Table 1). The referral rate for PDT to the RVI varied between health authorities. Newcastle Health authority had the highest rate of patients treated with PDT. The actual data are presented, plus an estimate based on the expected numbers requiring PDT throughout the region, assuming the incidence was the same as that in Newcastle.
A total of 82 patients were treated between January 2001 and December 2002, if the referral rate had been the same as that in Newcastle, up to 124 cases may be expected. This gives an annual incidence of 42 (up to 62) per 471 576 people over 65 in the Northern Region, from a total population of 2 899 146. This gives an incidence of 65 per 3 million. The population of the UK is about 60 million and so the annual incidence of second eye AMD patients who could be treated with PDT, assuming similar referral patterns, is 1300. Only two ‘second eye’ patients were treated, who were under 65 (64 and 62, not included in incidence calculations). The age range was 62–88, the average was 76. Five patients were treated for both eyes (included).
Included in the 82 patients were 15 who had a recurrence after focal argon laser. A detailed analysis of the PDT patients showing lesion type and lesion size is given in Table 2. We found that the visual acuity, measured with the 2 m EDTRS chart, had a variable correlation with Snellen acuity, so that a patient with 6/60 might see more or less than 34 logMAR letters, the cutoff for PDT in the TAP study. See Table 3 for the correlation of Snellen with logMAR for the TAP criteria patients treated with PDT. Table 4 gives the correlation of reading vision, using up to +4 D, and Snellen and logMAR.
An additional 21 patients had been treated for ‘second eye’ exudative AMD who were not eligible using the TAP criteria. Of these, 15 were <50% classic and six had <34 letters on refracted 2 m logMAR. Seven of the <50% classic lesions were small occult lesions, and thought worth treating in view of the severe loss of vision in the other eye and in view of the VIP study.6 One was more than 50% blood, but it was felt that the extent of the causative lesion was visible. Seven had been given the benefit of doubt when interpreting the FFA, but on retrospective review have been found to be less than 50% classic. The six with <34 letters had vision ranging from 25 to 33 letters, but on average only four letters in the other eye so thought worth treating. In all, 13 patients had ‘first eye’ treatment, two of whom subsequently developed ‘second eye’ involvement during the 2-year period. (These two are included in the 82.) In the vast majority of ‘second eye’ cases, vision in the ‘first eye’ had been lost due to macular degeneration. Other causes were amblyopia in four, injury in one and branch retinal vein occlusion in one.
In the study time period, PDT was also performed for the following causes of CNV: myopia 10; punctate inner choroidopathy six; peripapillary CNV three; choroidal rupture two; Sorsby's macular dystrophy two; angiod streaks one; Juxtafoveal telengectasia one.
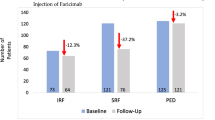
In 2002, 321 stereo FFAs were performed at the RVI for a provisional diagnosis of exudative AMD either in the hope of finding a treatable CNV or to confirm a diagnosis. The results are shown in Table 5. The RVI catchment area includes Newcastle and North Tyneside, Northumberland and some of Gateshead and County Durham, about 1 million with 200 000 over 65. The number performed for ‘second’ eyes was 181 and for ‘first’ eyes 140. The number of treatable ‘second eye’ patients based on FFA and visual acuity data, assuming ≥6/60 is equivalent to ≥34 logMAR letters (not always the case), was 36/181 (20%) and for ‘first eyes’ 20/140 (14%). Altogether, 30 of the ‘second’ eye patients went on to treatment; three being found to have <34 letters on 2 m logMAR testing and three were not referred on for treatment. In all but 17 (5%) of those who had an FFA, the visual acuity of the eye of interest was ≥6/60. There was no significant difference in the levels of visual acuity in the groups investigated for ‘first eye’ pathology compared to ‘second eye’. In total, 238 FFAs proved to be for exudative AMD. The total number of patients who were eligible for PDT using the TAP criteria was 50 (50/238=21%).
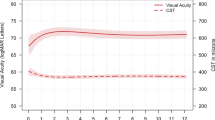
As of February 2003, 54, TAP criteria, AMD patients were 1 year from initial treatment. They had had refracted 2 m visual acuity using the EDTRS chart recorded at baseline and 1 year. In all, 12 had not made 1-year follow-up. Two had died and some were unwell. The average initial acuity, for those with follow-up data for 1 year, was 54.8 letters and at 1 year 43.5 (down 11.3). In all, 13 patients had lost more than 15 letters. See Figure 1 for 1-year follow-up visual acuity data. The responder rate defined as losing <15 letters was 42−13/42=69%. Seven of those who did not make 1-year follow-up had lost more than 15 letters when last seen. This would give a responder rate of 54−20/54=63%. The lowest confidence interval for outcome, assuming all the non-followed-up patients had lost >15 letters, would be 54−25/54=54%. Six patients had lost more than 30 letters including one not followed for the whole year (11%). None of those losing more than 30 letters did so within the first week of treatment, as is a potential risk of treatment.
Side effects from treatment were mild with low back pain being the only cause for concern; however, this settles if the patient walks around with the infusion running and certainly if the infusion is stopped. Back pain occurred in five cases. In one, the infusion was stopped. When the patient was retreated 3 months later, the back pain did not recur. Chest pain occurred in one patient, but was mild and stopped at the end of the infusion. We have had no cases of sunburn reported. All patients brought with them, or were supplied with, dark glasses, plus were advised to cover up or stay indoors for 48 h.
The average number of treatments was 3.2. One patient had one treatment; six had two; 15 had three; 17 had four; and three had five.
Discussion and conclusions
The incidence of patients who will present and be eligible for PDT in a population is unknown. This paper gives an estimate for the Northern region in the UK and leads on to give an estimate of 1300 ‘second eyes’ per year in the UK. There was a difference in referral rates for PDT from different health authorities in the Northern region. The RVI in Newcastle, the centre for treatment, had the highest number of patients treated per head of population over 65. Had referral rates been equal throughout the region, estimated numbers of patients receiving ‘second eye’ PDT in a year were 62. This is only an annual incidence of 0.013% in a population over 65.
The incidence figures for ‘first eye’ eligible patients are not accurate, as funding for treatment was variable. In all, 13 patients were treated in 2 years. From the FFA study, it appears likely that the numbers would be similar (30 and 20), although maybe the slightly lower number for ‘first eyes’ is real as some patients lose vision in one eye without noticing it at first. The total number of patients who may benefit from PDT following the TAP criteria may therefore be about 2000 in the UK.
These figures are clearly low compared to what had been hoped for PDT. A review by Bressler and Gills suggested that 20–30% of 200 000 cases of exudative AMD in the USA may be treatable.7 If this was so, assuming the population of the USA is 250 million and the incidence of exudative AMD is the same, 10 000–14 000 patients would be expected in the UK. Our figure, however, is in keeping with what has been found in Southampton in the UK, where, between August 2000 and April 2001, from a population of 570 000, only seven patients were treated.8
This study is not a population-based prevalence or incidence study, but a report on the number of patients who have actually been found to be eligible for PDT and received PDT with our present systems. At least in the Northern Region funding has not been a reason for treatment to be denied for the ‘second eye’. Factors that could have influenced this figure are: the prevalence of AMD in the population; nonpresentation for, or delays in, treatment; accuracy of interpretation of FFAs and measurement of visual acuity. These factors are discussed.
Accurate data on the prevalence of AMD in the Northern Region are not available. The population in the Northern Region is largely Caucasian. Only one patient treated was Asian. Many papers have studied the prevalence of AMD in Caucasian populations, but few have defined the forms of AMD and not in relation to PDT. The Framingham,9 Gisborne,10 Melton Mowbray,11 Beaver Dam,12 Blue mountains,13 and Rotterdam14 studies found an overall prevalence of AMD of 6.4–20.9% in populations aged over 43 years, with increasing prevalence with increasing age. The prevalence of late AMD in the Beaver Dam,12 Blue mountains,13 and Rotterdam studies14 was between 1.2 and 1.4% of the population less than 86 years. The definition of late AMD in these studies included neovascular and atrophic AMD. The Melton Mowbray study11 reported the prevalence of exudative AMD of 1.3% over 7 years, in a population aged 84–97 years, although the authors report that this is probably an underestimate. The incidence of exudative AMD over 5 years in the Beaver Dam study was 0.6 and in the Blue Mountain study it was 1.6%. The Salandra study15 in Italy reports a low incidence overall of 1.1% in the over 60 population, but the authors note that this may be due to the genetic isolation of the population. Low incidence of AMD has been noted in many ethnic groups including black populations in Africa and Barbados, and in Hispanics in colarado.16 There is no reason to think the prevalence of AMD is low in the Northern Region. The number of FFAs performed for exudative AMD in a year in the RVI (238) suggest that it is common. In Southampton, over a 2-month period, only 14 FFAs were performed.8
Nonpresentation or delays in the presentation and referral systems could have affected the number of patients treated with PDT. From the time of referral to our clinic to treatment, the average delay was 2–3 weeks; however, the time from development of first symptoms was very variable. Delays may have occurred at all steps of the way, from the patient seeking help, to the optometrist or General Practitioner to the primary Ophthalmologist. We found the our data on delays to treatment were not accurate enough to draw firm conclusions; however, there is not always a clearcut relation between the time of onset of symptoms and the amount of damage caused by a CNV. While some grow quickly, others appear to remain fairly stationary for some time. The appearance of the CNV on FFA may be a more accurate way of dating a CNV or at least predicting its response to treatment. With time there is more fibrosis and as the lesion grows there are larger areas of blocked fluorescence in the centre of the CNV. Larger lesions are also less likely to be eligible for treatment. Only 14 of the 75 (18%), with disc areas measured and eligible for treatment, were over two disc areas. Better patient education and fast-track referral systems might increase the number of patients eligible for PDT.
Our study of FFAs for exudative AMD confirm the impression that the percentage of patients with exudative AMD, who have a lesion eligible for PDT, is about 20%.7 In a study by Margherio et al, 36% of cases were found eligible for PDT based on the TAP criteria.17 Interestingly, in a study looking at FFAs in patients who had presented within a month of development of symptoms, only 8% were eligible, but 25% had extra or juxta foveal lesions and were eligible for focal argon laser.18 In this study, more patients were found who might benefit from PDT based on the VIP study6 (13%) rather than TAP. In our series, the incidence was a similar 21% with VIP and 20% with TAP. The VIP study recommendations are for eyes with progressive Type 1 occult lesions of <4 disc areas with a vision of ≤20/50 but ≥20/100.
The number of ‘first eye’ patients to ‘second eye’ eligible patients investigated was similar, suggesting that lack of funding for treatment did not stop investigation. This issue was addressed if treatment was found to be an option. It could be argued that some of our FFAs may not have been needed on clinical grounds; however, the indications were both to look for treatable patients and for diagnostic purposes. Only 17 (17/321=5%) were performed in patients with <6/60 vision, and so were unlikely to fit the treatment criteria on visual acuity grounds. Our study of FFAs does not give a measure of the number of patients who already had established disciforms, as usually an FFA is not performed for this. We do not have an accurate measure of these cases. A population-based prevalence study would be required.
The number of patients found suitable for extra/juxta foveal argon laser was small compared with some previous reports (7/238=3%). This may suggest that our patients presented relatively late, as a study by Grey et al found that 43% of eyes examined within 3 or 4 weeks after the onset of symptoms were amenable to laser treatment but only 10% after 5–6 months.19
The accuracy of interpretation of FFAs of course would influence our figures for eligible patients. Clearly, this is an issue for more borderline cases and will be for any service. Variability is found in reading FFAs.20 We retrospectively found that seven FFAs had been inaccurately assigned as >50% classic (7/95=7.3%). This level of inaccuracy does not significantly affect our overall incidence figures for the population.
The measurement of visual acuity could be a variable factor in defining the eligible population, as having a visual acuity of ≥34 letters was required for treatment. All our patients had a refracted 2 m logMAR visual acuity at baseline to allow comparison with TAP data for audit purposes. Snellen 6/60 is supposed to be equivalent to 34 letters on 2 m logMAR, but our results show that there is some variability in this. Reading vision also has a variable correlation (Tables 3 and 4). The exact way visual acuity is measured would therefore alter the number of patients found eligible for treatment. It may be that some patients with lower than 34 letters may still benefit from treatment in preserving what little vision they have or limiting the scotoma size.
Other aspects of the diagnosis of exudative AMD cases have not been addressed in our study of FFAs, as this did not effect the indications for PDT. ICGs were not routinely performed with all FFAs but were in selected cases for polypoidal choroidopathy, and to look for hot spots in occult lesions. Useful incidence figures are not possible with this data. Such diagnoses might, however, allow more patients to be treated.18
Approximately one-quarter (25) of the patients treated with PDT at the RVI did not have AMD. While the funding for PDT treatment for CNV secondary to AMD has still not been fully clarified by the National Institute for Clinical Excellence (NICE) at the time of writing, hence the ‘first eye’ ‘second eye’ distinction, funding for non-AMD cases, has not been addressed nationally.21 Some evidence for benefit is available in these cases, but due to their rarity a randomized controlled trial may not be possible. It may be only by performing the treatment and keeping a national record of outcome that an impression of benefit or otherwise be made in each condition. As a group, non-AMD CNV may provide a significant minority of the work load.
The outcome of our PDT treatment in AMD is in keeping with the results of the TAP study.2 At 1 year, 69% (29/42) lost <15 letters compared to 67% in TAP. Most patients lost some vision, as expected from the TAP study (Figure 1). Two patients gained >15 letters and an additional three gained five, nine and 12 letters, respectively. Follow-up for a 3-monthly treatment in an elderly population, especially if a centre covers a wide geographic area, is clearly a problem as 12/54 (22%) did not reach 1 year. This may partly be due to patients feeling the treatment was not worth it as they had lost vision. Indeed, 7/12 had lost >15 letters when last seen. If these seven are taken into account, the response rate would be 34/54=63%. If all these patients had lost >15 letters, the response rate would have been 29/54=54%. Illness and indeed mortality are also factors in this age group. Two of the patients had died.
No serious side effects from treatment occurred. Back pain occurred on five occasions, which is found to be relieved by the patient walking around with the infusion continuing, or, if absolutely necessary, stops with halting the infusion. Indeed, there are less side effects than from the FFA required. Six patients lost more than 30 letters, including one of the patients not followed for the full year (11% compared to 10% in TAP) but not within a week of treatment. The number of treatments required in a year were similar to TAP at 3.2 compared to 3.4 in TAP.
The numbers presented are too small to make any useful subgroup analysis into which factors other than those used to select patients may have led to a better result. The data have been supplied to the UK. PDT users group, who hope to collect data on outcome on all PDT treatment in the UK, so that a large data set can be collected to analyse the effect of this treatment.21
In conclusion, the number of patients eligible for PDT following the TAP criteria are not as large as might have been estimated; however, it does appear that the treatment works as well as it was claimed in the TAP study. It is to be hoped that, with better patient education and referral systems and with new treatments being developed, more patients with AMD will be helped.
References
Taylor HR, Keefe JE . World blindness: a 21st century perspective. Br J Ophthalmol 2001; 85: 261–266.
Bressler NM . Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with Verteporfin: one-year results of 2 randomised clinical trials-TAP report 1. Arch Ophthalmol 1999; 117: 1329–1345.
Bressler NM . Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with Verteporfin: two year results of 2 randomised clinical trials–TAP report 2. Arch Ophthalmol 2001; 119: 198–207.
Soubrane G, Bressler NM . Treatment of subfoveal choroidal neovascularisation in age related macular degeneration: focus on clinical application of vereporfin photodynamic therapy. Br J Ophthalmol 2001; 85: 483–495.
Macular photocoagulation study group. Subfoveal neovascular lesions in age-related macular degeneration. Arch Ophthalmol 1991; 109: 1242–1257.
Verteporfin in photodynamic therapy study group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization-verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001; 131: 541–560.
Bressler NM, Gills JP . Age related macular degeneration, new hope for a common problem comes from photodynamic therapy. Br Med J 2000; 321: 1425–1427.
Mandal N, Chisholm IH . Identifying the proportion of age related macular degeneration patients who would benefit from photodynamic therapy with verteporfin (Visudyne). Br J Ophthalomol 2002; 86: 118–119.
Kahn HA, Leibowitz HM, Ganley JP, Kini M M, Colton T, Nickerson RS et al. The Framingham Eye Study. I. Outline and major prevalence findings. Am J Epidemiol 1977; 106: 17–32.
Martinez GS, Campbell AJ, Reinken J, Allan BC . Prevalence of ocular disease in a population study of subjects 65 years old and older. Am J Ophthalmol 1982; 94: 181–189.
Dickinson AJ, Sparrow JM, Duke AM, Thompson JR, Gibson JM, Rosenthal AR . Prevalence of age-related maculopathy at two points in time in an elderly British population. Eye 1997; 11: 301–314.
Klein R, Klein BEK, Linton KLP . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Mitchell P, Smith W, Attebo K, Wang JJ . Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology 1995; 102: 1450–1460.
Vingerling JR, Dielemans I, Hofman A, Grobbee DE, Hijmering M, Kramer CF et al. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology 1995; 102: 205–210.
Pagliarini S, Moramarco A, Wormald RPL, Piguet B, Carresi C, Balacco-Gabrieli C et al. Age-related macular disease in rural Southern Italy. Arch Ophthalmol 1997; 115: 616–622.
Klein R, Klein BEK, Cruickshanks KJ . The prevalence of age-related maculopathy by geographic region and ethnicity. Prog Retin Eye Res 1999; 18: 371–389.
Margherio RR, Margherio AR, DeSantis ME . Laser treatments with verteporfin and its potential impact on retinal practices. Retina 2000; 20: 325–330.
Huddad WM, Coscas G, Soubrane G . Eligibility for treatment and angiographic features at the early stage of exudative age related macular degeneration. Br J Ophthalmol 2002; 86: 663–669.
Grey RB, Bird AC, Chisholm IH . Senile disciform macular degeneration. Features indicating suitability for photocoagulation. Br J Ophthalmol 1979; 63: 85–89.
Kaiser RS, Berger JW, William AG, Tolentino MJ, Maguire AM, Alexander J et al. Variability in fluorescein angiography interpretation for photodynamic therapy in age related macular degeneration. Retina 2002; 22: 683–690.
Harding S . Verteporfin photodynamic therapy in the UK: implications of the NICE appraisal. Eye 2003; 17: 119–121.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented in part at the Royal College of Ophthalmologists Annual Congress 2002
Rights and permissions
About this article
Cite this article
Talks, S., Setty, R. & Clarke, L. The incidence and outcome of photodynamic therapy for macular degeneration in the Northern Region of the UK. Eye 18, 588–594 (2004). https://doi.org/10.1038/sj.eye.6700709
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700709
Keywords
This article is cited by
-
Intravitreal bevacizumab in the treatment of neovascular age-related macular degeneration, 6- and 9-month results
Eye (2008)
-
The presentation of data relating to visual acuity
Eye (2007)
-
Polypoidal Choroidal Vasculopathy and Retinochoroidal Anastomosis in Japanese Patients Eligible for Photodynamic Therapy for Exudative Age-Related Macular Degeneration
Japanese Journal of Ophthalmology (2006)
-
One-year outcomes after photodynamic therapy in patients with age-related macular degeneration with poor baseline visual acuity
Graefe's Archive for Clinical and Experimental Ophthalmology (2006)
-
Influence of photodynamic therapy for age related macular degeneration upon subjective vision related quality of life
Graefe's Archive for Clinical and Experimental Ophthalmology (2006)