Abstract
Aim
To determine whether significant correlations exist between retinal sensitivity measured by fundus-related microperimetry and the visual acuity and the foveal thickness measured by optical coherence tomography (OCT) in eyes with diabetic macular edema (DME).
Methods
A retrospective chart review of 32 eyes with DME and 17 normal healthy eyes that had undergone fundus-related microperimetry and OCT. The macular sensitivity was measured using the recently introduced fundus-related microperimeter, Micro Perimeter 1. The mean retinal sensitivities within the central 2° and 10° were correlated with the best-corrected visual acuity and OCT-measured foveal retinal thickness.
Results
The mean sensitivities in the central 2° and 10° were significantly lower in patients with DME than in normal subjects (P<0.0001). The mean retinal sensitivities in the central 2° and 10° were inversely correlated with visual acuity (r2=0.623, P<0.0001; r2=0.581, P<0.0001) and foveal thickness (r2=0.581, P<0.0001; r2=0.551, P<0.0001).
Conclusions
The mean retinal sensitivities measured with fundus-related microperimetry were significantly lower in eyes with DME than in normal eyes. Because a significant correlation of the microperimeter-determined retinal sensitivity to visual acuity and foveal thickness was observed, the retinal sensitivities obtained by fundus-related microperimetry may be another measure that can be used to assess the effects of DME.
Similar content being viewed by others
Introduction
It has been established that fundus-related perimetry is clinically useful for the assessment of macular function.1, 2, 3, 4, 5 Microperimetry with a scanning laser ophthalmoscope (SLO) has long been the only commercially available fundus perimeter, but because it was not equipped with an automated eye tracking system, it was not easy to examine patients in a routine clinical setting.
The recently introduced fundus-related microperimeter, MP1 (Nidek, Japan), can be used to obtain quantitative and reliable measurements of retinal sensitivity by tracking eye movements while the patient is focused on a fixation target. This system uses a high-speed tracking software which monitors fundus movements to ensure that the anatomic landmarks revealed in the fundus photographs are precisely aligned with the sensitivity maps generated by the perimeter.6, 7 This instrument allows the overlaying of retinal sensitivities onto a real-colour fundus image to indicate the retinal areas where visual defects coincide with visible structural anomalies. It was recently reported that the perimetric results from MP1 are comparable to those obtained with SLO-microperimetry.6
The purpose of our study was to measure the sensitivity of the macula with the MP1 in patients with diabetic macular edema (DME), and to compare the perimetric results with the best-corrected visual acuity (BCVA) and the foveal retinal thickness measured by optical coherence tomography (OCT).
Subjects and methods
The medical charts of 32 eyes of 25 patients with clinically significant macular edema as defined by the Early Treatment Diabetic Retinopathy Study8 or cystoid macular edema (CSME) were reviewed. The age of the patients ranged from 25 to 76 years (58.8±11.8 years; mean±SD). All patients underwent a complete ophthalmic examination, including indirect ophthalmoscopy, fluorescein angiography, and BCVA. Fluorescein angiography did not show ischemic maculopathy in any of the diabetic eyes, and none of the eyes had macular photocoagulation. In all, 17 subjects, ranging in age from 42 to 76, without ophthalmic abnormalities comprised the normal control group.
This study followed the tenets of the Declaration of Helsinki, and informed consent was obtained from all subjects after the nature and possible consequences of the study were explained.
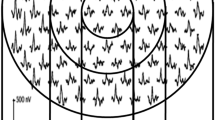
Fundus-monitored microperimetry was performed with the Micro Perimeter 1 (MP1, Nidek, Japan). The MP1 software contains an automatic tracking system for fundus movements that evaluates every acquired frame for shifts in the x- and y-directions of the fundus with respect to a reference frame obtained by an infrared camera at the beginning of the examination. A 4-2-staircase strategy with Goldmann III size stimulus was used, and 24 stimulus locations covering the central 10° were examined by microperimetry (Figure 1). The white background illumination was set at 1.27 cd/m2. The differential luminance, defined as the difference between stimulus luminance and background luminance, was 127 cd/m2 at 0 dB stimulation, and the maximum stimulus attenuation was 20 dB. The duration of the stimulus was 100 ms, and a 12° cross was used as the fixation target. The mean retinal sensitivities at the 4 locations covering the central 2° and at 24 locations covering the central 10° were determined.
The retinal thickness was defined as the distance between the vitreoretinal interface and the retinal pigment epithelium in the centre of the fovea, that is, the foveola, using the Stratus OCT 3000 (Carl Zeiss Meditec, Dublin, CA, USA).
The numerical data were analysed using Mann–Whitney's U test. A P-value of <0.05 was considered statistically significant.
Results
The BCVA (in log MAR units), foveal thickness, and mean retinal sensitivity for the 4 central points and 24 points measured with the MP1 are presented in Table 1. The mean BCVA was significantly reduced in DME eyes (P<0.0001), and the mean OCT-determined foveal thickness was significantly thicker in DME eyes (P<0.0001). The mean retinal sensitivities at both the central 4 points and at the 24 points were also significantly lower in DME eyes than in normal eyes (P<0.0001).
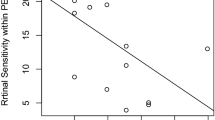
Scatter plots of the BCVA (log MAR units) as a function of the mean retinal sensitivity of the central 4 points (A) and the 24 points (B) for each of the DME patients (closed circles) and normal subjects (open circles) are shown in Figure 2. There was a significant correlation between the BCVA and the mean retinal sensitivity of the central 4 points (r2=0.623, P<0.0001) and the 24 points (r2=0.581, P<0.0001).
(a) Relationship between mean retinal sensitivity of 4 points covering the central 2° and best-corrected visual acuity in logMAR units for each of the DME patients (closed circles) and normal subjects (open squares). The linear regression line for all subjects is y=0.909–0.061x (r2=0.623, P<0.0001). (b) Relationship between mean retinal sensitivity of the central 24 points covering the central 10° and best-corrected visual acuity with the same symbols as in (a). The linear regression line for all subjects is y=0.972–0.063x (r2=0.581, P<0.0001).
Scatter plots of the foveal thickness as a function of the mean retinal sensitivity at the central 4 points (A) and at the 24 points (B) for each of the DME patients and normal subjects are shown in Figure 3. For all of the data, a significant negative correlation was also observed between the foveal thickness and the mean retinal sensitivity of the central 4 points (r2=0.581, P<0.0001) and that of 24 points (r2=0.551, P<0.0001).
(a) Relationship between mean retinal sensitivity of the 4 points covering the central 2° and foveal thickness for each of the DME patients (closed circles) and normal subjects (open squares). The linear regression line for all subjects is y=583.8–27.3x (r2=0.581, P<0.0001). (b) Relationship between mean retinal sensitivity of the central 24 points covering the central 10° and foveal thickness with the same symbols as in (a). The linear regression line for all subjects is y=613.6–28.2x (r2=0.551, P<0.0001).
Discussion
These results demonstrated that the retinal sensitivity in the macular area measured by the MP1 is significantly correlated not only with the visual acuity but also with the foveal thickness in DME patients. Previous studies have shown that the OCT-determined foveal thickness was significantly correlated with the BCVA in eyes with DME.9, 10, 11 In many patients with macular diseases, however, the visual acuity is not necessarily related to foveal or macular function, mainly because eyes with poor foveal function often use eccentric fixation.
We have examined the macular function by using multifocal electroretinography (mfERG), and found that the electrical responses obtained from the macular area were also significantly correlated with the foveal thickness.11, 12 The results indicated that the mfERGs may provide an objective method to evaluate and assess DME.
There have been several papers reporting that microperimetry using SLO measures the local retinal function effectively in eyes with DME.4, 5 Rohrschneider et al4 studied changes in retinal sensitivity after laser treatment for CSME using their original software for automated static threshold perimetry with SLO. They also reported that retinal sensitivity and fixation stability were more reduced in CSME patients than with normal controls. Mori et al5 detected a macular scotoma in 74% patients with CSME, and found that the scotoma was related to the cystoid changes and the type of macular edema. Since the degree of macular edema was determined by stereoscopic fundus examinations and fluorescein angiography in both studies, the direct correlation between foveal thickness and retinal sensitivity has never been evaluated.
Recently, the microperimetric results obtained by SLO and MP1 were compared, and it was reported that the major disadvantage of the MP1 was the low quality of the first acquired black-and-white infrared image used for eye tracking during examination.6 This resulted in artifacts within the centre of the infrared image, which makes detection of retinal pathology and test pattern placement unreliable. Another reported disadvantage was that the MP1 did not allow for the addition of stimuli after the beginning of the examination, so that the exact delineation of a scotoma was missed when there were no stimulus points within the macular lesion. However, because the MP1 is equipped with real-time fundus tracking and colour images of the fundus, this instrument provided comparable perimetric results as SLO microperimetry.6
In conclusion, retinal sensitivity of the macular area determined by the MP1 was significantly correlated with visual acuity and with morphological changes revealed by OCT. The combination of OCT and MP1 can be easily performed in routine clinical settings, and may provide other methods to evaluate and assess DME.
References
Timberlake GT, Mainster MA, Webb RH, Hughes GW, Trempe CL . Retinal localization of scotomata by scanning laser ophthalmoscopy. Invest Ophthalmol Vis Sci 1982; 22: 91–97.
Sjaarda RN, Frank DA, Glaser BM, Thompson JT, Murphy RP . Assessment of vision in idiopathic macular holes with macular perimetry using the scanning laser ophthalmoscope. Ophthalmology 1993; 100: 1513–1518.
Rohrschneider K, Gluck R, Becker M, Holz FG, Kruse FE, Fendrich T et al. Scanning laser fundus perimetry before laser photocoagulation of well-defined choroidal neovascularisation. Br J Ophthalmol 1997; 81: 568–573.
Rohrschneider K, Blültmann S, Glück R, Kruse FE, Fendrich T, Völcker HE . Scanning laser ophthalmoscope fundus perimetry before and after laser photocoagulation for clinically significant diabetic macular edema. Am J Ophthalmol 2000; 129: 27–32.
Mori F, Ishiko S, Kitaya N, Hikichi T, Sato E, Takamiya A et al. Use of scanning laser ophthalmoscope microperimetry in clinically significant macular edema in type 2 diabetes mellitus. Jpn J Ophthalmol 2002; 46: 650–655.
Rohrschneider K, Springer C, Blültmann S, Völcker HE . Microperimetry – comparison between the Micro Perimeter 1 and scanning laser ophthalmoscope – fundus perimetry. Am J Ophthalmol 2005; 139: 125–134.
Shah VA, Chalam KV . Liquid crystal display microperimetry in idiopathic subretinal fibrosis. Ophthalmic Surg Lasers Imag 2004; 35: 321–324.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Arch Ophthalmol 1985; 103: 1796–1806.
Hee MR, Puliafito CA, Duker JS, Reichel E, Coker JG, Wilkins JR et al. Topography of diabetic macular edema with optical coherence tomography. Ophthalmology 1998; 105: 360–370.
Otani T, Kishi S, Maruyama Y . Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol 1999; 127: 688–693.
Yamamoto S, Yamamoto T, Hayashi M, Takeuchi S . Morphological and functional analyses of diabetic macular edema by optical coherence tomography and multifocal electroretinograms. Graefe's Arch Clin Exp Ophthalmol 2001; 239: 96–101.
Yamamoto S, Yamamoto T, Ogata K, Hoshino A, Sato E, Mizunoya S . Morphological and functional changes of the macular after vitrectomy and creation of posterior vitreous detachment in eyes with diabetic macular edema. Doc Ophthalmol 2004; 109: 249–253.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okada, K., Yamamoto, S., Mizunoya, S. et al. Correlation of retinal sensitivity measured with fundus-related microperimetry to visual acuity and retinal thickness in eyes with diabetic macular edema. Eye 20, 805–809 (2006). https://doi.org/10.1038/sj.eye.6702014
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702014
Keywords
This article is cited by
-
Retinal ultrastructural, electrophysiological, and microvascular morphological outcomes in diabetic macular edema treated with intravitreal bevacizumab
Irish Journal of Medical Science (1971 -) (2023)
-
Correlation of macular sensitivity measures and visual acuity to vision-related quality of life in patients with age-related macular degeneration
BMC Ophthalmology (2021)
-
Impacts of intravitreal anti-VEGF therapy on retinal anatomy and neurophysiology in diabetic macular edema
International Ophthalmology (2021)
-
Structural and functional findings in patients with moderate diabetic retinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Visual rehabilitation via microperimetry in patients with geographic atrophy: a pilot study
International Journal of Retina and Vitreous (2017)