Abstract
Aims
To develop a methodology for case-mix adjustment of surgical outcomes for individual cataract surgeons using electronically collected multi-centre data conforming to the cataract national data set (CND).
Methods
Routinely collected anonymised data were remotely extracted from electronic patient record (EPR) systems in 12 participating NHS Trusts undertaking cataract surgery. Following data checks and cleaning, analyses were carried out to risk adjust outcomes for posterior capsule rupture rates for individual surgeons, with stratification by surgical grade.
Results
A total of 406 surgeons from 12 NHS Trusts submitted data on 55 567 cataract operations between November 2001 and July 2006 (86% from January 2004). In all, 283 surgeons contributed data on >25 cases, providing 54 319 operations suitable for detailed analysis. Case-mix adjusted results of individual surgeons are presented as funnel plots for all surgeons together, and separately for three different grades of surgeon. Plots include 95 and 99.8% confidence limits around the case-mix adjusted outcomes for detection of surgical outliers.
Conclusions
Routinely collected electronic data conforming to the CND provides sufficient detail for case-mix adjustment of cataract surgical outcomes. The validation of these risk indicators should be carried out using fresh data to confirm the validity of the risk model. Once validated this model should provide an equitable approach for peer-to-peer comparisons in the context of revalidation.
Similar content being viewed by others
Introduction
Cataract surgery is the most frequently performed surgical procedure in the NHS, with 332 625 operations having been reported for 2009–2010 in England, a crude surgical rate of around 6.65/1000 population.1 Ophthalmology departments generally and cataract units in particular are well advanced in the adoption of electronic working practices with ∼40% of English NHS Trusts using electronic patient record systems as part of routine cataract care. The NHS Information Standards Board has recently approved the Cataract National Data set (CND) as an ‘Inherited Data Standard’, which should underpin and facilitate further uptake of electronic working in cataract surgery.2 Routine standardised electronic data collection in the context of a high-volume surgical procedure and a widely accepted intra-operative surgical benchmark quality indicator makes cataract surgery an ideal candidate for the development and piloting of a methodology for case-mix adjustment of outcomes.
Based on analysis of 55 567 cataract operations, our group has reported updates and benchmarks on surgical practice across a range of issues including patient demographics, preoperative visual acuity, anaesthesia, anticoagulants, surgical complications, risk indicators for posterior capsule rupture, ocular biometric properties, visual acuity outcomes and variations in unadjusted posterior capsule rupture rates for individual surgeons.3, 4, 5, 6, 7, 8 Of particular relevance to the present report is our previous finding that based on routine preoperatively collected data, the predicted probability of a complication during surgery may vary by 100 fold from 0.75% for the most straightforward lowest-risk cases to over 75% for the highest-risk most complex cases.5 Furthermore the grade of surgeon has an important influence on the likelihood of a complication arising.9
Transparency of medical and surgical outcomes has become a matter of public concern, with the medical director of the NHS having indicated a clear expectation that in the future the clinical outcomes of individual surgeons will be placed in the public domain.10, 11 The issue is therefore no longer whether this will or will not occur, it is now a question of which form it should take. Risk adjustment of outcomes for case complexity has been in use in cardiac surgery for a number of years.12
The aim of this report is to outline a methodology for case-mix adjustment of surgical outcomes for individual cataract surgeons using electronically collected preoperative multi-centre data conforming to the cataract national data set (CND).
Method
Risk indicators for the benchmark intra-operative surgical complication, posterior capsule rupture or vitreous loss or both (abbreviated in this paper as PCR) have previously been published for this population of cataract operations.5 For the purposes of this report, we repeated the previous multivariate logistical regression analysis with inclusion of information on paired eyes to acknowledge within patient inter-eye correlation. Using risk profiles based on patient and eye indicators applicable to individual operations, a risk score was calculated in the form of a composite odds ratio for each operation. From the statistical model a predicted probability of a complication was derived as described in our earlier report.5 For each surgeon contributing >25 procedures an average case complexity profile was calculated as the mean of the predicted probabilities for PCR across all of that surgeon's cases and this information is presented graphically for all surgeons. As an initial step, based on both this summary measure of the surgeon's case complexity and the grade of the surgeon, the expected complication rate for the cases undertaken was compared directly with each surgeon's actual observed complication rate, the results being presented graphically as the difference between observed and expected rates. Finally, to allow fairer comparison against an average or benchmark rate, complication rates for each surgeon have been adjusted for case complexity.13 To make such adjustment, with placement of confidence limits around the results, the statistical methodology we have used involves construction of funnel plots with the observed/expected rate for each surgeon on the vertical axis against the expected number of complications (PCR events) on the horizontal axis.14 As output from this method may not be intuitively accessible to surgeons unfamiliar with this statistical approach, we have placed a secondary horizontal axis above each plot as an aid to interpretation of the funnel plots. The secondary horizontal axis shows the approximate surgical volume based on the average PCR rate for the relevant surgical group, which is more similar to our previously published unadjusted results.4 In this way separate plots have been presented for: (1) all contributing surgeons (this analysis includes adjustment for grade of surgeon); (2) independent surgeons (consultants, associate specialists, staff grade surgeons); (3) senior trainee surgeons (fellows, specialist registrars) and; (4) junior trainee surgeons (designated as senior house officers at the time of data collection, now first or second year specialty registrars (ST1 and ST2).
A local ethics committee confirmed that ethics approval was not required, as this work was an audit and no patients, hospitals or healthcare workers were identifiable.
Results
There were 283 surgeons with data on >25 cataract operations, together providing data for analysis on a total of 54 319 operations. Inclusion of information on paired eyes to acknowledge any within patient inter-eye correlations improved statistical rigour, with results remaining essentially unchanged from our previously published logistic regression model.5
Case complexity description
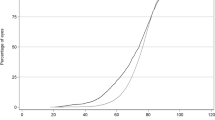
Based on the model the average case complexity (predicted probability of PCR from patient factors) for each of the 283 individual surgeons appears in Figure 1, the average predicted probability of a complication varied between 2.62 and 1.17%.
Following inclusion of the risk associated with the surgeon's grade, the arithmetic difference between observed PCR rate and expected rate is plotted against surgical volume in Figure 2 for all 283 surgeons. It is of note that towards the left where samples are small there is a wide vertical spread, which reflects statistical sampling error for small samples.
Difference between observed PCR rate and expected PCR rate for 283 surgeons contributing N>25 cases, total N=54 319 operations. Positive % values indicate a rate higher than that expected (poorer than expected performance), negative values indicate better than expected performance. The wide spread to the left demonstrates uncertainty where number of cases is small.
Case complexity adjustment and confidence limits
Results are presented as a series of case-mix adjusted funnel plots with each point on the plots representing an individual surgeon's case-mix adjusted results set in the context of their peers and with 95 and 99.8% confidence limits. Figure 3 shows all 283 surgeons with results corrected for both case complexity and grade of surgeon, the overall PCR rate being 1.92%. Figures 4, 5 and 6 show the three grades of surgeon separately, 108 independent surgeons, 140 senior trainees, 35 junior trainees, with results adjusted for case complexity alone and the relevant group PCR average rates taken into account (1.41, 2.48 and 5.1% respectively). On the basis of statistical sampling error it would be expected that 95% of surgeons’ results would lie inside the inner pair of confidence limits with 2.5% above and 2.5% below. Similarly for the outer pair it would be expected that 0.1% (∼1/1000) would lie above and 0.1% below these lines.
Adjusted funnel plot for all surgeons: ratio of observed to expected number of operations complicated by PCR vs expected number of complications for each of 283 surgeons. Risk adjustment accounts for patient characteristics and grade of surgeon. A secondary ‘x-axis’ above the plot indicates the approximate volume of cases based on the overall PCR rate=1.92% (total N=54 319 operations).
Adjusted funnel plot for independent surgeons: ratio of observed to expected number of operations complicated by PCR vs expected number of complications for 108 independent surgeons. A secondary ‘X-axis’ above the plot indicates the approximate volume of cases based on the overall PCR rate=1.41% (N=36 485 operations).
Adjusted funnel plot for senior trainee surgeons: ratio of observed to expected number of operations complicated by PCR vs expected number of complications for 140 senior trainee surgeons. A secondary ‘X-axis’ above the plot indicates the approximate volume of cases based on the overall PCR rate=2.48% (N=15 277 operations).
Adjusted funnel plot for junior trainee (SHO) surgeons: ratio of observed to expected number of operations complicated by PCR vs expected number of complications for 35 junior trainee surgeons. A secondary ‘X-axis’ above the plot indicates the approximate volume of cases based on the overall PCR rate=5.1% (N=2557 operations).
Discussion
This work pilots a methodology for case-mix adjustment of cataract surgical outcome for the benchmark intra-operative complication of PCR. The methodology is applicable to high-volume medical work with discrete well-defined outcomes. The methodology requires an initial analysis of a large (statistically powerful) set of data in order to identify the risk indicators for outcomes of interest. The rarer the outcome the larger the database required. In terms of this analysis for cataract surgery, our risk model requires validation on a fresh set of data, which we intend to do as a ‘next step’, and looking ahead to the future, all similar health-related risk models should be validated on a regular basis to maintain currency. Our results include descriptions of the overall case-mix risk profiles for each of the 283 surgeons who contributed >25 cases towards the 54 319 cases included in these analyses. On the basis of the patient and eye risk indicators (without adjustment for the grade of operating surgeon), the predicted probabilities for PCR ranged from 2.62% for the surgeon with the most complex overall case mix to 1.17% for the surgeon with the least.
We have chosen >25 cases as the case volume cut off on the basis that an expected number of complications of <0.5 becomes intuitively meaningless as actual complications arise in integer values, and furthermore confidence limits cannot be computed for expected numbers <1 (on the graphical presentations the confidence limits stop at expected number of complications=1). The wide scatter associated with low numbers of cases is illustrated in all the funnel plots presented here. In the absence of a statistically robust method for assessment of complication rates when the number of cases is small, a common sense approach is required. This may for example take the form of a pragmatically chosen rate for low volumes of surgery by an individual surgeon. In the context of appraisal for independent surgeons such an approach would facilitate discussion where deskilling because of low surgical volume was potentially a problem, and would also provide a ‘safety net’ for detection of a possible poor performer undertaking occasional surgery. The rate chosen for low-volume surgery would of necessity be somewhat arbitrary and would need to acknowledge the surgical circumstances so that for established surgeons a slightly different approach would be needed compared with trainees. A candidate for the chosen threshold could be the rate of the upper confidence interval where the line ends towards the left side of the plot (ie, where the expected number of complications=1; Obs/Exp=9.2; Observed Rate=1.41 × 9.2=13%).
This methodology allows the work of individual surgeons to be seen in the context of their peers, both for trainees and established independent surgeons. Confidence limits on the case-mix adjusted funnel plots provide the fairest available method for identification of surgical outliers. In the setting of a surgical procedure where the predicted probability of a complication is estimated to vary by as much as 100 fold depending on patient characteristics, adjustment for case complexity of the case mix of individual surgeons is essential for credible comparisons between surgeons. It should be remembered that with all such analyses statistical sampling error will play a role and it is therefore important to bear this in mind when interpreting such data. In terms of identification of poor performance, a surgeon whose results lie above the upper confidence limits has a probability of being in these extreme upper positions of 2.5 and 0.1%, respectively. Although potentially alarming, such results for individual surgeons must be expected from time to time to arise purely as a result of chance. Interpretation of such results is beyond the scope of this paper but it may be reasonable to suggest that criteria for an amber alert might be outside the upper 95% limit (probability 2.5% or 1 in 40) and for a red alert outside the upper 99.8% limit (probability 0.1% or 1 in 1000), with such alerts based on well defined case-mix adjusted outcomes and analysed separately according to grade of surgeon. On the other hand the opposite tails (the other 2.5 and 0.1%) would be of interest in terms of identification of outstandingly good performers from whom lessons in good practice may be gained.
Increasing expectations on the part of the public have stimulated discussion around the need for transparency in terms of quality of services, including quality of surgical outcomes. In the NHS cardiac surgeons have led the way11, 12, 13 in the wake of well-publicised failures of surgical care. The advent of electronic patient records for routine collection of detailed standardised data items brings fresh opportunities for in depth analysis of specific outcomes including risk indicators for adverse outcomes. These developments open the door to a range of quality improvement opportunities, for example early identification of higher-risk cases to ensure that more risky operations are performed by the most highly skilled surgeons. In the context of revalidation, expected to commence in 2012, the ability to undertake continuous electronic audit will significantly reduce the burden on surgeons to provide evidence of ongoing competence. Case complexity is believed to be a significant determinant of outcome in many medical fields but until recently detailed high-quality information with sufficient statistical power to quantify these risk indicators has been unavailable. Our previous and current work illustrate both the importance and the feasibility of risk adjustment when attempting comparisons between surgeons. Appropriate case-mix adjustment of outcomes should alleviate potential concerns on the part of those highly skilled surgeons who take on higher risk complex cases. Without risk adjustment there is the possibility that surgeons may become risk aversive when offering surgery, with the unwanted consequence that patients, who may otherwise benefit from surgery, could be denied access because of a surgeon's concerns about being adversely judged should a complication arise.
Conclusions
In this paper, we present a methodology for risk adjustment of PCR rates in cataract surgery applicable to individual surgeons. Regular validation of the underpinning risk model should be undertaken to maintain relevance. The methodology has applicability to other fields of high-volume medical and surgical work with discrete outcomes. Properly audited and risk-adjusted surgeon's results will have value in the contexts of fairly judged revalidation and quality assurance for the public.

References
HESonline. Main procedures and interventions. http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=205, 2010.
ISB. The Information Standards Board for Health and Social Care. http://www.isb.nhs.uk/documents/isb-0085/amd-156-2010/index_html, 2010.
Knox Cartwright NE, Johnston RL, Jaycock PD, Tole DM, Sparrow JM . The Cataract National Dataset electronic multicentre audit of 55 567 operations: when should IOLMaster biometric measurements be rechecked? Eye (Lond) 2010; 24: 894–900.
Johnston RL, Taylor H, Smith R, Sparrow JM . The Cataract National Dataset electronic multi-centre audit of 55 567 operations: variation in posterior capsule rupture rates between surgeons. Eye (Lond) 2010; 24: 888–893.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM et al. The Cataract National Dataset electronic multicentre audit of 55 567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye 2009; 23: 31–37.
Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Galloway P et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye 2009; 23: 38–49.
El-Hindy N, Johnston RL, Jaycock P, Eke T, Braga AJ, Tole DM et al. The Cataract National Dataset Electronic Multi-centre Audit of 55 567 operations: anaesthetic techniques and complications. Eye 2009; 23: 50–55.
Benzimra JD, Johnston RL, Jaycock P, Galloway PH, Lambert G, Chung AK et al. The Cataract National Dataset electronic multicentre audit of 55 567 operations: antiplatelet and anticoagulant medications. Eye 2009; 23: 10–16.
Sparrow JM . Cataract surgery: benchmarks for established and trainee surgeons. Eye (Lond) 2008; 22: 1371–1372.
Keogh B . Outcome Measurement in Surgery. The case, the tools and the timing. The Royal College of Surgeons of England. Meeting 27 May 2008, oral presentation.
Keogh B, Spiegelhalter D, Bailey A, Roxburgh J, Magee P, Hilton C . The legacy of Bristol: public disclosure of individual surgeons’ results. BMJ 2004; 329: 450–454.
Bridgewater B, Keogh B, Kinsman R, Walton P . The Society for Cardiothoracic Surgery in Great Britain & Ireland. Sixth National Adult Cardiac Surgical Database Report. http://www.scts.org/documents/PDF/Sixth_NACSD_report_2008_with_c.pdf, 2008.
Spiegelhalter DJ . Funnel plots for comparing institutional performance. Stat Med 2005; 24: 1185–1202.
ERPHO. The association of public health observatories: spreadsheet for producing funnel plots for ISR/SMRs. http://www.apho.org.uk/resource/item.aspx?RID=25353, 2008.
Acknowledgements
We are grateful to all the ophthalmologists who contributed data to this survey, without whose support it would not have been possible. This work was supported by a grant from the Academy of Medical Royal Colleges entitled ‘Developing a defensible decision making algorithm for revalidation based on case-mix adjusted measures of surgical performance’, which was administered through the Royal College of Ophthalmologists.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Robert Johnston is a Director of Medisoft Limited.
Additional information
Sections of this work have been presented at: (1) The Royal College of Ophthalmologists Annual Congress, May 2010. (2) The Academy of Medical Royal Colleges, December 2010.
Rights and permissions
About this article
Cite this article
Sparrow, J., Taylor, H., Qureshi, K. et al. The cataract national data set electronic multi-centre audit of 55 567 operations: case-mix adjusted surgeon's outcomes for posterior capsule rupture. Eye 25, 1010–1015 (2011). https://doi.org/10.1038/eye.2011.103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.103
Keywords
This article is cited by
-
Graphical comparison of surgeon outcomes for the audit of a national corneal transplant registry (OTAG study 32)
Eye (2023)
-
A data-driven approach to evaluate factors affecting resident performance in cataract surgery
International Ophthalmology (2023)
-
Intraoperative head drift and eye movement: two under addressed challenges during cataract surgery
Eye (2018)
-
The evaluation of the risk factors for capsular complications in phacoemulsification
International Ophthalmology (2018)
-
United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: Report 1; Case mix, complications, and cataract
Eye (2013)