Abstract
Aims National blindness surveys conducted in the Gambia in 1986 and 1996 showed an increase in blindness and visual impairment from non-trachomatous opacity. This study aimed to investigate the aetiology of these opacities and to assess the resulting visual burden.
Methods A population-based, randomised blindness survey was conducted in the Gambia in 1996. Patients with visual impairment or blindness were examined by an ophthalmologist with a slit lamp. Causes of corneal opacity were determined as accurately as possible by clinical history and examination.
Results A total of 154 patients with non trachomatous corneal opacity were examined of whom 39 had bilateral opacities and 115, unilateral. Causes included corneal infection, measles/vitamin A deficiency, harmful traditional practices and trauma (unilateral scarring). Overall, corneal pathology alone was responsible for bilateral visual impairment or blindness in 19 (12%) patients and unilateral visual impairment or blindness in 88 (57%) patients. Those patients with bilateral visual impairment or blindness (mean age 59, SD) were older (P = 0.003) than others (mean age 44, SD = 20). The use of harmful traditional eye practices was associated with bilateral corneal blindness or visual impairment (RR = 2.63, 95% CI 1.11–6.21, P = 0.04). Although none of the corneal scars reported here were attributed to trachoma, in patients over the age of 45, the prevalence of trachomatous conjunctival scarring in this group was 38.8% compared to 19.4% of the whole nationwide sample.
Discussion Strategies for the prevention (including the quest for cheaper anti-microbial drugs and co-operation with traditional healers) and surgical treatment of these corneal opacities are discussed.
Similar content being viewed by others
Introduction
Corneal scarring is known to be a leading cause of blindness in Africa.1,2,3 National surveys of blindness and visual impairment in the Gambia conducted in 1986 and 1996 showed a reduction in the age-standardized prevalence of blindness from 0.60% to 0.42%, a relative reduction of 30%. This included an 80% relative reduction in trachomatous blindness.4 In contrast blindness due to non-trachomatous corneal opacity has increased from 11% in 1986 to 17% in 1996 when it was the second leading cause of blindness. The estimated number of persons blind from non-trachomatous corneal opacities increased 33% from 600 to 800 over the 10-year period. This trend of increased prevalence of non-trachomatous corneal opacity compared to trachomatous corneal opacity has also been demonstrated in other developing countries.5,6,7 Non-trachomatous corneal opacity therefore warrants close attention from national eye care planners seeking to reverse this trend. Previous data concerning this type of disease in African populations are few. This paper describes the series of patients identified in the 1996 survey as having non-trachomatous corneal opacity and analyses demographic characteristics, aetiological factors, and visual morbidity for such cases.
Methods
A population-based randomised sampling method was used as has been described elsewhere.8
The fieldwork was undertaken using three teams, each working in a different part of the country after standardization. A two-part ophthalmic examination included measurement of visual acuity in all subjects with, and without, pinhole correction and a basic anterior segment examination, performed by an ophthalmically trained nurse. Any person with a visual acuity of less than 6/18 in either eye was referred for detailed examination by one of three ophthalmologists (including HF) to determine the cause or causes of visual impairment. Blindness was defined by the World Health Organization criteria9 as corrected vision of less than 3/60 in the better eye; low vision was vision less than 6/18 but at least equal to 3/60 in the better eye. The presence or absence of a ‘central corneal opacity’ was recorded, requiring part of the opacity to overlie at least part of the pupillary axis. Aetiology of corneal opacity was ascribed on the basis of history and examination. Corneal opacity was regarded as non-trachomatous if there was no trichiasis or signs of epilation present and no history of trichiasis. If trichiasis was present but there was a clear history of the corneal opacity developing before the trichiasis and the position of the corneal scar did not correspond to the trichiasis, then the corneal opacity was regarded as non-trachomatous. If trachomatous scarring was present on the tarsal conjunctiva (TS) but there was no evidence of past or present trichiasis then the corneal opacity was regarded as non-trachomatous.
With regard to specific aetiologies of non-trachomatous corneal opacities, trauma, surgery, traditional eye medicine use or measles were often specifically cited as causes by the patients; others were clear that they had been born with the problem. A unilateral red painful eye prior to development of the scar was generally thought to indicate an infective corneal ulcer. On examination, measles often causes bilateral central corneal scars; inferior symblepharon is often the result of harmful traditional eye medicine; evidence of previous surgery or couching was sometimes helpful.
Results
Demography
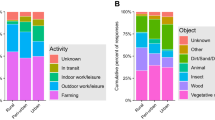
A total of 13046 (92% of the calculated sample of 14110) people were examined. One hundred and fifty-four patients with non trachomatous corneal opacity were identified, 39 of whom had bilateral opacities and 115, unilateral. Eighty-one patients (53%) were male and 73 (47%) were female. Mean age was 46 years (SD = 21, range 0–97). Distribution of unilateral and bilateral corneal opacity by age-group is illustrated in Figure 1.
Aetiology
Tables 1 and 2 show the aetiologies of the corneal opacities for unilateral and bilateral cases. The miscellaneous category included degenerative conditions such as pterygium and spheroidal degeneration as well as corneal dystrophies. Trauma caused only unilateral opacity whereas congenital/neonatal aetiology, measles/vitamin A deficiency and unknown aetiologies were all more commonly bilateral. Sex of patient was not significantly associated with aetiology.
Visual status
Visual acuities were measured in 153 patients, the remaining patient being unable to comply with testing but not believed to be blind.
(a) Bilateral cases (n = 39)
As shown in Table 1, 17 (44%) patients had normal vision, 14 (36%) patients had visual impairment (though in two of these additional pathology, other than corneal, contributed to the impairment in one eye: phthisis in one and cataract in another) and 8 patients (20%) were blind. The blindness was judged due to the corneal pathology in both eyes of all 8 patients. Aetiology was not significantly associated with visual status in bilateral cases.
(b) Unilateral cases (n = 115)
Table 2 shows visual status of the eye with the corneal opacity using the World Health Organization definitions of unilateral visual impairment (visual acuity of less than 6/18 but at least equal to 3/60) and blindness (visual acuity less than 3/60). Only those patients in whom the corneal opacity was judged to be the chief cause of the visual impairment in the eye are included in the visually impaired and blind categories for the purposes of this table. Corneal infection was significantly associated with visual impairment/blindness in unilateral cases (RR = 1.43, 95% CI 1.14–1.80, P = 0.022). Of the 48 patients who were blind in the eye with corneal opacity, 11 (23%) were also blind in the other eye from another cause, cataract and phthisis being the two common causes. Fifteen patients with unilateral opacity were bilaterally visually impaired, again cataract and phthisis being the common diagnosis in the other eye.
Overall, corneal pathology alone was responsible for bilateral visual impairment or blindness in 19 (12%) patients and unilateral visual impairment or blindness in 88 (57%) patients. Those patients with bilateral visual impairment or blindness (mean age 59, SD = 18) were older (P = 0.003) than others (mean age 44, SD = 20).
Harmful traditional practices
These were judged the prime cause of the corneal opacities in a total of nine cases, four couchings and five from traditional medication. The latter practice was also felt to be an additional secondary factor in 14 other cases (in these cases there was clear clinical evidence of another cause of corneal scar which may have provoked the use of traditional practices), making a total of 23 (15%) in which traditional practices contributed to corneal damage. There were no significant differences in age and sex between those 23 and the rest. The use of such harmful traditional eye practices was associated with bilateral corneal blindness or visual impairment (RR = 2.63, 95% CI 1.11–6.21, P = 0.04) as illustrated in Table 3. This association remained significant whether or not the couching cases were included.
Trachomatous conjunctival scarring
None of the corneal opacities in this study were attributed to trachoma, by definition. Trachomatous corneal opacity found in the survey has been reported elsewhere.3 Nevertheless 53 (34.4%) patients had signs of trachomatous conjunctival scarring on lid eversion and 14 (9.1%) of these had some degree of trichiasis. These are much higher than the general population prevalences of scarring (4.9%) and trichiasis (0.9%). If patients over the age of 45 only are included, the prevalence of scarring in this group was 38.8% compared to 19.4% of the whole nationwide sample, and the prevalence of trichiasis was 8.8% compared to 4.6% of the nationwide sample. Table 4 illustrates that trachomatous scarring was particularly associated with bilateral corneal opacity (RR = 2.22, 95% CI 1.30–3.89, P = 0.006). This association remained if cases with trichiasis were excluded. There was no significant association between presence of trachomatous scarring or trichiasis and aetiology of corneal opacity.
Discussion
Non-trachomatous corneal opacity is now the second leading cause of blindness in the Gambia accounting for an estimated 800 blind people and 1200 visually impaired people throughout the country. Another 1100 people are estimated to be blind and 1500 visually impaired from non-trachomatous corneal opacity in one eye and another cause (usually cataract or phthisis) in the other, making a total of 4600 in whom corneal opacity contributes to some degree of visual impairment. This compares to estimates of 3800 people with trachomatous corneal opacity and 300 with blinding trachomatous corneal opacity.4
It is not always possible, even for experienced ophthalmologists using slit lamps, to judge the cause of corneal scarring retrospectively. This is an inherent problem in investigating corneal opacity and limits the precision of the aetiological data presented here and accounts for the large number of patients in the survey without known aetiology. Prospective studies would give more accurate data but would be logistically very difficult to perform. In the absence of such studies, the methods presented here (the examination of a population-based sample by trained ophthalmologists experienced in African ophthalmology, who then make a retrospective clinical judgement as to aetiology where possible) at least give a basic estimate of the contributions of various aetiological factors to this problem. In this study it was harder to attribute specific aetiologies to bilateral cases. Of the aetiological categories which were identified, the most common was corneal infection, followed by trauma, then measles/vitamin A deficiency, and then harmful traditional practices including couching.
Corneal infection or ulceration due to bacteria, viruses and fungi has been widely reported in African countries.10,11 Reports from developing countries suggest that risk factors for corneal ulceration involve minor trauma such as abrasions and foreign bodies in about 50–70% of cases and ocular surface disorders in 20–30%. In this study trachomatous scarring was associated with bilateral corneal opacity but not specifically with corneal infection. A major problem is delay in presentation of minor corneal trauma and early infection, despite the existence of several regional health centres with well trained eye nurses throughout every division of the Gambia (which is thought to have accounted for a major part of the overall reduction in blindness). Specific education aimed at encouraging earlier presentation of such cases is required. Another problem is that the best chemotherapeutic agents for treating corneal ulcers, especially fungal ulcers, are expensive and often not readily available at district level. Trials are presently underway in the search for cheaper antibacterial agents which could be made more available to those in need. Malaria, which is endemic in the Gambia, has been shown to predispose to herpes simplex keratitis11 and it is possible that campaigns to provide insecticide-impregnated bed nets might reduce the prevalence of this cause of corneal opacity.
Another possible reason for late presentation of such cases is that they sometimes prefer to visit a traditional healer or to self medicate with substances such as herbal washings (cassava and mango leaves were common choices). In addition, an estimated 2400 people in the Gambia show evidence of harmful traditional practices having contributed towards their corneal opacity and harmful traditional practices were significantly associated with bilateral visual impairment or blindness. Traditional practices have previously been implicated in corneal ulceration in Africa12 and with poor visual outcome13 and their association with corneal visual impairment/blindness in the Gambia is important. This finding highlights the need to seek opportunities to co-operate with and to train traditional healers, which has shown initial promise in Malawi,14 as well as continuing to educate the general public about the possible dangers of traditional practices.
Trauma was another large aetiological group, causing only unilateral disease but important since nearly a quarter of patients blind in one eye from unilateral corneal opacity were blind in the other eye from another cause. There was no association between traumatic aetiology and age or sex in this study, though a similar study in Tanzania found that traumatic corneal opacity was more common in men. In Gambian society women are very active agriculturally and therefore are exposed to the same risks of trauma. Efforts should be made towards education about safe working practice and early presentation to health facilities after accidents. Good visual results are sometimes achievable with appropriate surgical management of anterior segment trauma even if the lens is involved and despite the delays in presentation inevitable in an African context.15
Vitamin A deficiency and/or measles was thought to be responsible for corneal opacity in an estimated 1200 patients. Vitamin A-rich foods such as mango, papaya, oily fish and red palm oil are readily available throughout the Gambia and nutritional education together with a measles immunisation programme which already reaches 97% of the population should see this problem decreasing in the future.
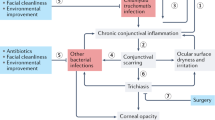
The fact that patients with corneal opacity are more likely than the general population to have trichiasis is not surprising but the association with uncomplicated trachomatous conjunctival scarring has not previously been reported. It is possible that similar environmental risk factors contribute to both diseases but that does not fit with the dramatic reduction of trachomatous blindness alongside the increase in non-trachomatous blindness. Trachomatous scarring, by its effects on conjunctival goblet cells and their ductules, Meibomian glands and even the lacrimal gland, can produce dry eye disease,16,17 predisposing to corneal infection and perhaps, through discomfort, to the use of traditional eye medicine. It is also conceivable that trachomatous scarring alters the natural bacterial flora, hence predisposing to corneal infection. Trachomatous scarring is invariably bilateral and was associated specifically with bilateral corneal opacities in this study, suggesting that conjunctival scarring may play a part in the aetiology of corneal scarring. Whatever the mechanism of the association, national eye care planners targeting prevention of corneal blindness strategies can note that areas of the Gambia known to have a high prevalence of trachomatous scarring may also have an even higher prevalence of ‘non-trachomatous’ corneal opacity. There is currently a World Health Organization campaign for the global elimination of trachoma as a public health problem by the year 2020 (GET2020) by promotion of the SAFE strategy (Surgery for trichiasis, Antibiotics for active disease, Facial cleanliness and Environmental improvement).18 The impact of community trachoma control programmes on the prevalence of non-trachomatous corneal opacity warrants further investigation.
Although the emphasis should be on prevention of corneal opacity, surgical treatment may be appropriate. Optical iridectomies, if there is enough clear inferior peripheral cornea, and pterygium excisions can be performed at regional health centres. Penetrating keratoplasty is not currently performed in the Gambia. A recent report from Kenya19 demonstrated good visual results from this operation with certain limited diagnoses, ie keratoconus and corneal dystrophies which did not account for large numbers of patients in this series. Meticulous post-operative care of the eye in addition to regular hospital follow up for at least a year are required for successful rehabilitation following penetrating keratoplasty, neither of which may be feasible for the majority of rural patients reported in this series.
In summary the results reported here emphasise the need to continue to increase accessibility to both health education, with particular attention to the role of traditional practices, and eye care services in order to ensure that blindness and visual impairment from corneal disease follows the downward trend of other blinding eye diseases in the Gambia.
References
Chirambo MC, Tizazu T . Ocular disease and ophthalmic services in Malawi. Soc Sci Med 1983; 17: 1773–1780
Whitfield R, Schwab L, Bakker NJ, Bisley GG, Ross DD . Cataract and corneal opacity are the main causes of blindness in the Samburu tribe of Kenya. Ophthalmic Surg 1983; 14: 139–144
Cook CD, Knight SE, Crofton-Briggs I . Prevalence and causes of low vision and blindness in northern KwaZulu. S Afr Med J 1993; 83: 590–593
Dolin PJ, Faal H, Johnson GJ, Ajewole J, Mohamed AA, Lee PS . Trachoma in the Gambia. Br J Ophthalmol 1998; 82: 930–933
Moll AC, van der Linden AJ, Hogeweg M, Schader WE, Hermans J, de Keizer RJ . Prevalence of blindness and low vision of people over 30 years in the Wenchi district, Ghana, in relation to eye care programmes. Br J Ophthalmol 1994; 78: 275–279
Zhang SY, Zou LH, Gao YQ, Di Y, Wang XD . National epidemiological survey of blindness and low vision in China. Chin Med J Engl 1992; 105: 603–608
Brilliant LB, Pokhrel RP, Grasset NC et al. Epidemiology of blindness in Nepal. Bull World Health Organ 1985; 63: 375–386
Faal H, Minassian DC, Dolin PJ, Mohamed AA, Ajewole J, Johnson GJ . Evaluation of a national eye care programme: re-survey after 10 years. Br J Ophthalmol 2000; 84: 948–951
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th revision WHO: Geneva 1992 pp 456–457
Hagan M, Wright E, Newman M, Dolin P, Johnson G . Causes of suppurative keratitis in Ghana. Br J Ophthalmol 1995; 79: 1024–1028
Yorston D, Foster A . Corneal ulceration in Tanzanian children: relationship between malaria and herpes simplex keratitis. Trans R Soc Trop Med Hyg 1992; 86: 456–457
Yorston D, Foster A . Traditional eye medicines and corneal ulceration in Tanzania. J Trop Med Hyg 1994; 97: 211–214
Mselle J . Visual impact of using traditional medicine on the injured eye in Africa. Acta Trop 1998; 70: 185–192
Courtright P, Lewallen S, Kanjaloti S . Changing patterns of corneal disease and associated vision loss at a rural African hospital following a training programme for traditional healers. Br J Ophthalmol 1996; 80: 694–697
Bowman RJ, Yorston D, Wood M, Gilbert C, Foster A . Primary intraocular lens implantation for penetrating lens trauma in Africa. Ophthalmology 1998; 105: 1770–1774
Blodi BA, Byrne KA, Tabbara KF . Goblet cell population among patients with inactive trachoma. Int Ophthalmol 1988; 12: 41–45
Tabbara KF, Bobb AA . Lacrimal system complications in trachoma. Ophthalmology 1980; 87: 298–301
Global elimination of blinding trachoma. Resolution WHA 51.11 adopted by the World Health Assembly 16 May 1998 Text at http://www.who.int/pbd/trachoma/wha51-e.htm
Yorston D, Wood M, Foster A . Penetrating keratoplasty in Africa: graft survival and visual outcome. Br J Ophthalmol 1996; 80: 890–894
Acknowledgements
The authors wish to thank Dr AA Mohammed, Dr J Ajewole, Mr PS Lee and other members of the survey team. The survey was funded by Sight Savers International and the British Council for the Prevention of Blindness.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
This article is cited by
-
Bilateral congenital choanal atresia and osteoma of ethmoid sinus with supernumerary nostril: a case report and review of the literature
Journal of Medical Case Reports (2011)