Abstract
Purpose To assess the effect of an intervention comprising training in optic disc assessment, explicit referral criteria and ophthalmologist feedback on referred patients, on the number of optometrist referrals for suspected glaucoma seen at a referral site and the positive predictive value of those referrals.
Methods Optometric practices routinely referring to the Ealing Hospital Eye Clinic were randomly divided into two groups taking into consideration those practices, which shared an optometrist (a cluster) and the number of optometrist days worked per week. One group of practices acted as controls, while the other practices were invited to receive the intervention. Data on 397 new patients referred and presenting to Ealing Hospital with suspected glaucoma were collected over a 20-month period. The data on patients who had failed to attend their appointment were collected over 7 months of this period. The number of referrals seen, the positive predictive value of those referrals, and the attendance rate were calculated. Optometrist's opinions of the intervention were assessed qualitatively. Data relating to optometrist compliance with the intervention were also collected.
Results The number of glaucoma referrals presenting to Ealing Hospital from the intervention practices was almost double that from the control practices (210 vs 119). When cluster randomisation, the number of optometrist days per cluster and the number of assessed referrals in the preintervention period are taken into consideration, it is estimated that the intervention is associated with a 52% increase in the number of referrals reaching Ealing Hospital. However, the design effect resulting from the cluster randomisation was unexpectedly high (of the order of 13–14) and so the confidence intervals around the estimate of 52% are very wide (95% c.i. 35% decrease to 253% increase, P=0.34). There was no evidence of an association between optometrist compliance with the intervention and the number of referrals seen at Ealing Hospital. The positive predictive value (PPV) of referrals was similar for the intervention (0.49 (95% c.i. 0.42, 0.55)) and control groups (0.46 (95% c.i. 0.33, 0.60)). Optometrist opinions of the intervention were largely favourable. All expressed a willingness to participate in future programmes.
Conclusion A large difference in the number of referrals between the practice groups was observed. Since the PPV of referral was unchanged, the potential impact of the intervention in terms of numbers of new cases of glaucoma detected in the community is substantial. However, because of its large design effect, this trial does not provide conclusive evidence of an impact of the intervention on referral numbers. A considerably larger trial will be required to produce conclusive evidence of an effect.
Similar content being viewed by others
Introduction
Primary open angle glaucoma (POAG) is a chronic optic nerve neuropathy with a reported prevalence of just under 2% in a UK Caucasian population aged over 50 years.1 Prevalence is strongly age-related. POAG is the leading cause of preventable blindness in the UK, accounting for 12% of blind registrations and 9.6% of partial sight registrations.2 Because of under-registration, the true figures are likely to be significantly greater.3
Glaucoma progresses slowly and patients are usually unaware of having the condition until it becomes advanced.4 Treatment can only prevent further damage and is most commonly aimed at reducing the intraocular pressure (IOP). There is no formal screening programme for glaucoma in the UK, so detection is largely dependent on the public attending an optometrist for sight testing, with optometrists responsible for over 90% of referrals to the Hospital Eye Service.5,6,7,8 Three tests/examinations are recommended for the detection of glaucoma; measurement of IOP, visual field and optic disc assessment. However, optometrist case-finding and referral criteria vary considerably across the profession.9,10 Over the past decade, there has been a shift in practice with increasingly large numbers of patients being referred on the basis of optic disc appearance and/or visual field loss with less emphasis on IOP.11
Recent studies have reported positive predictive values (PPV) of optometrist referrals for glaucoma ranging between 0.31 and 0.50.5,7,9,11,12,13,14 As PPV is directly related to prevalence and prevalence is low, this figure implies that optometrist referrals have a high degree of specificity.15
The proportion of undetected glaucoma in the developed world, however, remains at about 50%.1,16,17 Several approaches have been proposed to try to reduce this proportion within the UK. These include the use of referral guidelines11 and the use of repeat examination by accredited optometrists.18 We conducted a randomised controlled trial to test an intervention aimed at improving optometrist case-finding through training in optic disc assessment, the provision of explicit referral criteria and ophthalmologist feedback on referred patients. To our knowledge, this was the first time such a study had been undertaken.
Methods
Prior to this study, the PPV of referrals to the Ealing Hospital eye clinic had been assessed and has been reported elsewhere.9
Optometrist population
The trial was conducted in optometric practices routinely referring via general practitioners (GPs) to Ealing Hospital. A letter was sent to every local optometric practice requesting information regarding the names of the optometrists and the number of days worked per week. Practices that employed only ophthalmic medical practitioners (OMPs) were excluded from the study. Optometric practices grouped into clusters, a cluster being a group of practices that shared an optometrist. There were 25 such clusters in the trial area. These clusters were then divided into two groups, those with up to 10 optometrist days per week and those with more than 10 days per week. Within each group, half of the optometric clusters were randomly selected to receive the intervention using computer-generated random numbers. The remaining clusters acted as control clusters. Control clusters received no intervention. Each optometrist working at intervention group practices was invited to participate in the study.
The intervention
The intervention comprised three components.
-
1
Training in optic disc assessment: Optic disc changes precede field defects19 and current optic disc assessment by optometrists is often restricted to the evaluation of only two parameters.9,10 Thus a major aim of the intervention was to improve the discrimination of glaucomatous from normal discs by encouraging the adoption of a more thorough and systematic evaluation of the optic nerve head. A pilot study was conducted (with a separate population of optometrists to the trial population) to test the proposed method of disc assessment. The accuracy of reporting each of nine disc parameters and the validity of the proposed method at discriminating glaucomatous from normal discs were evaluated. The findings, reported elsewhere,20 resulted in a procedure based on the assessment and interpretation of seven parameters (see Box 1). Training of optometrists was provided initially through two 1 hour lectures. Well-defined criteria for normal and glaucomatous appearances for each parameter were discussed. Structured forms listing the seven parameters were provided to facilitate utilisation of the new method. The optometrists were asked to complete a structured form for each patient examined aged over 34 years, and to send these forms to the investigators. These forms enable us to estimate the proportion of glaucoma referrals actually seen at Ealing Hospital.
Box 1 Parameters used for optic nerve head assessment -
2
Provision of standardised referral criteria: Large local variations exist in the provision of referral criteria for glaucoma case-finding. Referral guidelines have been shown to be beneficial in other studies.21 Therefore, a set of referral criteria for suspected glaucoma cases was provided to all optometrists in intervention clusters.
-
3
Ophthalmologist feedback to optometrists: Poor communication between ophthalmologists and optometrists regarding referrals remains a problem despite the obvious learning benefits and potential improvements in quality of referrals.22,23 Therefore, replies were sent to each referring optometrist in the intervention clusters, detailing the ophthalmologist's findings, diagnosis and management plan for each patient who presented to Ealing Hospital eye clinic.
To encourage compliance and to reduce drop-out, on-going training was provided through a series of lectures and practical sessions held at four to five monthly intervals for the duration of the study. Personalised invitations were sent to each intervention-randomised optometrist in advance of every lecture irrespective of previous attendance. Staff changes were monitored through an annual review process. New staff were invited to participate in the trial and the initial training was repeated.
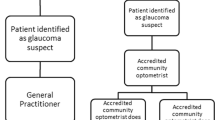
Referral path
The referral path for a patient from the optometrist to the Ealing Hospital eye clinic and the ways in which referred patients may be ‘lost’ are shown in Figure 1. For the sources of the numbers in the different compartments of the figure (A2–5, B2–5), see below. These numbers are derived from the disc assessment forms completed by the optometrists in the intervention group.
Outcome evaluation
A referral for suspected glaucoma was defined as any concern relating to IOP and/or disc excavation, and/or field defect excepting disc appearances or field defect that the optometrist had attributed to other pathology. All patients presenting to Ealing Hospital with a glaucoma referral from any of the optometric practices in the trial were evaluated by one of 10 ophthalmologists. The optometrists in the intervention group were unaware of whether their referrals were being analysed. At the end of the trial period, one consultant (with a special interest in glaucoma) (IM) reviewed all the notes and using information recorded at the initial clinic visit, made a diagnosis. All ophthalmologists were unaware as to which group the referring optometrist belonged.
Patients were classified as confirmed glaucoma, suspected glaucoma or not glaucoma. For the purposes of PPV calculation, a positive outcome was defined as a confirmed or suspected diagnosis of glaucoma, where the term glaucoma encompasses open angle, closed angle and secondary glaucoma. Open angle glaucoma (OAG) was defined as pathological optic disc changes compatible with glaucoma in the presence of an open angle on gonioscopy and in the absence of any other ocular finding associated with secondary glaucoma. The definitions for all the diagnostic categories including normals and ocular hypertensives have been reported previously.9 A patient was treated as a suspect if s/he was felt to warrant repeat examination or follow-up to clarify the diagnosis.
The impact of the intervention was assessed by examining the numbers of referrals for suspected glaucoma from intervention and control practices and the positive predictive value of those referrals.
Patients already diagnosed with glaucoma were excluded from the analysis. Patients referred for other conditions (eg cataract) and subsequently found to have glaucoma (missed glaucoma) were also excluded from analysis.
Over a 7-month period (June 2000–January 2001) the number of patients, referred by their optometrist with suspected glaucoma, and referred on to Ealing Hospital by their GP who failed to attend for their appointment was identified from clinic records (B4, Figure 1). At the end of the data collection period, an attempt was made to interview by telephone each optometrist in the intervention group to obtain their opinions on the intervention. An interviewer who was unfamiliar with the optometrists conducted all interviews and the responses were made anonymous. The Moorfields Ethical Committee granted ethical approval for the entire study.
Data analysis
Analysis was performed on a pragmatic ‘intent to intervene’ basis. The numbers of referrals seen at Ealing Hospital was calculated for each cluster of practices in the trial. These were compared between intervention and control clusters using the Poisson regression, with the logarithm of the number of optometrist days per cluster as an offset in the model and assuming random (gamma-distributed) cluster effects. The positive predictive value of referrals in the intervention and control groups was compared using and additive risk model and the GEE approach to take account of the cluster randomisation.
Results
A total of 32 practices in 25 clusters were identified for inclusion in the study. At the start of the study, 16 practices (13 clusters, 24 optometrists) were randomised to the intervention group leaving 16 practices (12 clusters, 29 optometrists) in the control group (Figure 2). Over the course of the trial, practices in both groups used locum optometrists and had temporary posts and changes of staff. By the second half of the trial, seven optometrists had left the intervention group and six had left the control group.
Table 1 presents a comparison of the intervention and control practices with respect to number of optometrist days per week, practice type, and experience at baseline. The groups were broadly similar with respect to the number of optometrists involved and their experience, the number of days worked per week and type of practice. During the 6-month period from September 1996 to February 1997, prior to the start of the trial, 53 patients referred with suspected glaucoma from trial practices were assessed at Ealing Hospital. Roughly, equal numbers from intervention and control practices were assessed (Table 1).
In total, 19/24 (79%) of those optometrists in the intervention group practices at the start of the study attended the initial training sessions on disc assessment. Attendance at six subsequent sessions ranged between 40 and 50%. Three optometrists did not attend any of the lectures. Six optometrists moved away during the course of the study and one retired and closed his practice. Seven replacement optometrists were identified and invited to participate in the intervention. Three attended the repeated initial training lecture.
Ten optometrists who worked in the intervention practices (32%) sent in disc assessment forms of whom four sent in forms covering time periods greater than 10 months. In all, 2877 forms were sent in by optometrists working at the intervention practices during the course of the study. Of these patients, 100 (3.5%) (A2, Figure 1) were referred with suspected glaucoma of whom 49 (49%) (A4, Figure 1) were referred on by their GP to the Eye Unit at Ealing Hospital. Eight of these (16%) did not attend their hospital appointment (B4, Figure 1).
Attendance rates
Table 2 suggests a higher attendance rate (82%) among individuals referred by the intervention practices and onwards by their GPs than among individuals referred by the control practices (70%). However, when account is taken of the clustered nature of the data, there is no evidence that this difference is not a chance finding (P=0.46).
Of the 21 individuals from control practices who failed their appointment, 19 were referred from practices in Southall, giving a nonattendance proportion of 19/43=44% for that area. This compares with 2/27 (7%) for the remaining control practices and 16/87 (18%) for intervention practices.
Number of referrals presenting to Ealing Hospital
During the 20-month data collection period from August 1999 to March 2001 inclusive, 397 patients referred for suspected glaucoma were assessed at Ealing Hospital. Of these patients, 329 had been referred from practices in the trial (intervention and control) and were therefore eligible for inclusion in the study. Table 3 shows the number of referrals from the intervention practices seen at Ealing Hospital from each cluster. The number of assessed referrals from the intervention practices was almost double that from the control practices (210 vs 119). Taking account of the cluster randomisation, the number of optometrist days per cluster and the number of assessed referrals in the preintervention period, we estimate that the intervention was associated with a 52% increase in the number of referrals (95% c.i. 35% decrease to 253% increase, P=0.34). Since referral compliance appeared to be particularly low for optometrist practices in Southall, we also repeated the analysis excluding the Southall practices. This increased the estimated impact of the intervention to 79% (95% c.i. 29% decrease to 349% increase) because, paradoxically, these were practices from which high numbers of referrals were seen.
For the intervention practices, we generated a compliance score based on whether the optometrists had attended the first lecture, the proportion of all lectures they had attended and the number of months during which they submitted forms. We found no convincing evidence of an association between this compliance score and the number of referrals (P=0.13)
Similar proportions of individuals referred from the intervention and control practices had referring IOPS <22 (46% from intervention practices, 53% from control practices, P=0.7).
Positive predictive value
Overall, 102/210 of all assessed referrals from the intervention group resulted in a positive outcome (PPV=0.49 (95% c.i. 0.42–0.55)). The PPV for referrals was similar in the control group (55/119, PPV=0.46 (95% c.i. 0.33–0.60); difference=3%(95% c.i −9% to +15%)).
When the PPV was investigated by subtype, referrals for suspected normal-tension and suspected high-tension glaucoma, there was still no indication of difference in PPV between the intervention and control groups (data not shown).
Optometrist opinions of intervention
In total, 13 optometrists gave their opinions about the intervention. The majority of the optometrists were happy with the timing, length, frequency, and content of the lectures, although more practical training sessions were requested. All reported adopting a more comprehensive analysis of the optic disc and finding the forms useful, although time-consuming, to complete. Reference to referral criteria was rare for most respondents. Optometrists reported reading all ophthalmologist replies. All 13 optometrists expressed a willingness to participate in future intervention programmes. Better communication between the optometrists and the ophthalmologists was also cited as a positive effect of the intervention.
Discussion
To our knowledge, this is the first controlled trial of an intervention to increase optometrists’ referral of glaucoma patients. Our results are inconclusive. When designing the study, the sample size was calculated with the aim of detecting an increase in the PPV of glaucoma referrals from intervention practices. We found no evidence of such an increase. Tantalisingly, there is a suggestion that the intervention may have led to a substantial increase in the number of referrals. In the absence of any decline in the PPV of the referral, this implies an increase in the number of glaucoma cases identified by optometrists. Such an increase could be the result of an improvement in the sensitivity with which optometrists detect glaucoma cases or an increase in the number of undiagnosed glaucoma cases who visit optometrists. Such an effect, if real, would be of great public health importance. However, an unexpectedly large design effect (of the order of 13–14), resulting from the necessary use of cluster randomisation, means that our results are embedded in very wide confidence intervals and hence inconclusive.
The PPV of referrals is dependent on the prevalence of glaucoma in the population visiting optometrists and the validity (sensitivity and specificity) of the case-finding approach adopted by the optometrists. For a low-prevalence condition such as glaucoma, specificity has a more profound effect on the PPV than sensitivity because the majority of individuals are nondiseased.
Increasing the numbers of parameters assessed has the potential to increase screening sensitivity (more cases detected) but also decrease specificity (more false-positive findings), and thus the PPV in the intervention group might be expected to be lower than that in the control group. The absence of any substantial difference in PPV suggests that a high specificity was maintained by the intervention (the sensitivity could have increased substantially and the specificity decreased slightly or the intervention led to an increase in the proportion of those with undiagnosed glaucoma attending the intervention optometrists (and the specificity and/or sensitivity decreased). More informed and careful interpretation of clinical findings might result in a high specificity being maintained. However, we cannot exclude the possibility that the intervention optometrists told patients about the trial and this encouraged other individuals who suspected that they had glaucoma to present for testing.
The additional training in disc assessment might have been expected to increase the proportion of referrals that were for suspected normal-tension glaucoma. This, however, did not occur to any detectable extent. When the PPV was investigated by subtype (normal-tension/high-tension glaucoma), there was still no important difference between the intervention and control groups. Further analysis is required to investigate this and other aspects of referral quality and is beyond the scope of this paper.
Although proportionately more of those referred from intervention practices attended for review at hospital, this finding could be due to chance or could be the result of bias. The proportion of referred individuals not attending from Southall practices (controls) was appreciably greater than for the remaining control practices and the intervention practices. Southall has a large Indian population. It is possible that language barriers and cultural differences influence attendance rates. By chance neither of the two practice clusters in Southall were randomised to the intervention group. A fifth of total optometrist days per week in the control group were spent in practices in Southall.
In a recent qualitative study of patients awaiting hospital review following referral for suspected glaucoma, a lack of anxiety was found. This was put down to a lack of knowledge about glaucoma, reassurance by the long wait for a hospital appointment and a relative down-playing of the findings by the optometrist.24 In addition, public health knowledge of glaucoma is poor.4 A study within the Indian community in Ealing revealed public knowledge of eye disease to be extremely low. (D Patel and IE Murdoch, Barriers to uptake of eye care services by the Indian population living in Ealing, London. 2002, personal Communication).
It is unknown whether those not attending are more or less likely to have glaucoma than those who do attend. It might be argued that those with glaucoma affecting their sight and those with a family history are more likely to attend, hence the PPV may be higher in those attending than among all referrals.
The collection of disc assessment forms from the intervention group revealed that only 49% of referrals for suspected glaucoma were subsequently referred to Ealing Hospital. Again area may be a source of bias. Over 90% of the completed forms were from practices located within central Ealing. Since this is a large commercial center, it is possible that more of the patients attending these optometric practices had travelled some distance and live outside the area. The true proportion of referrals seen at Ealing Hospital from all study practices may be greater than 49%. Incomplete/unequal ascertainment of referral outcomes from both groups remains a potential source of bias in this study. It is, however, very likely to be nondifferential bias.
The results of this study are based on outcomes from all randomised practices irrespective of the level of compliance. Potential problems for the intervention were staff turnover and maintaining interest over time. An attempt was made to limit these by regular monitoring of staff changes, inviting new optometrists to participate and ongoing training. Attendance at the initial training lecture was high (79%) but dropped following the introduction of the disc assessment forms. Only 32% of optometrists sent in assessment forms, although this reflects a minimum estimate of compliance with the new disc assessment method; others may have used the method but not completed the assessment forms or not sent them in.
Vernon found that dissemination of referral guidelines made no appreciable difference to guideline adherence by optometrists.11 Our telephone interviews similarly indicated our referral guidelines were only referred to on an occasional basis.
In conclusion, our study suggests that the intervention may have increased the number of individuals referred by optometrists for suspected glaucoma. Since the PPV was unchanged, the potential impact in terms of numbers of new cases of glaucoma detected in the community is substantial. However, because of the necessary use of cluster randomisation and an unexpectedly large resultant design effect, our sample size was insufficient to provide a conclusive answer. We believe this finding to be of great potential public health importance. A much larger study is required to investigate this finding.
References
Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P . Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol 1993; 77: 17–21.
Evans JR . Causes of Blindness and Partial Sight in England and Wales 1990–1991 Studies on Medical and Population Subjects, No. 57. HMSO: London, 1995.
Bunce C, Evans J, Fraser S, Wormald R . BD8 certification of visually impaired people. Br J Opthalmol 1998; 82: 72–76.
Green J, Siddal H, Murdoch IE . Learning to live with glaucoma: a qualitative study of the diagnosis and impact of sight loss. Soc Sci Med 2002; 55: 257–267.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR . An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol 1994; 1: 31–39.
Bell RWD, O’Brien C . Accuracy of referral to a glaucoma clinic. Ophthalmic Physiol Opt 1997; 17(1): 7–11.
Newman DK, Anwar S, Jordan K . Glaucoma screening by optometrists: positive predictive value of visual field testing. Eye 1998; 12: 921–924.
Pooley JE, Frost EC . Optometrists’ referrals to the hospital eye service. Ophthalmic Physiol Opt 1999; 19: 16–24.
Theodossiades J, Murdoch IE . Positive predictive value of optometrist-initiated referrals for glaucoma. Ophthalmic Physiol Opt 1999; 19: 62–67.
Vernon SA, Henry DJ . Do optometrists screen for glaucoma?. Eye 1989; 3: 131–134.
Vernon SA, Ghosh G . Do locally agreed guidelines for optometrists concerning the referral of glaucoma suspects influence referral practice?. Eye 2001; 15: 458–463.
Bell RWD, O’Brien C . The diagnostic outcome of new glaucoma referrals. Ophthalmic Physiol Opt 1997; 17(1): 3–6.
Vernon SA . The changing pattern of glaucoma referrals. Eye 1998; 12: 854–857.
Wormald R, Rauf A . Glaucoma screening. J Med Screen 1995; 2: 109–114.
Murdoch IE, Theodossiades J . Is review of enriched populations the way forward for glaucoma case detection? Eye 2003; 17: 5–6.
Tielsch JM, Katz J, Singh K, Quigley HA, Gottsch JD, Javitt J et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am J Epidemiol 1991; 134: 1102–1110.
Mitchell P, Smith W, Attebo K, Healey PR . Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology 1996; 103: 1661–1669.
Henson DB, Spencer AF, Harper R, Cadman EJ . Community refinement of glaucoma referrals. Eye 2003; 17: 21–26.
Quigley HA, Green WR . The histology of human glaucoma cupping and optic nerve damage: clinicopathologic correlation in 21 eyes. Ophthalmology 1979; 86: 1803–1830.
Theodossiades J, Murdoch IE . What optic disc parameters are most accurately assessed using the direct ophthalmoscope? Eye 2001; 15: 283–287.
Lomas J, Anderson GM, Domnick-Pierre K . Do practice guidelines guide practice? N Engl J Med 1989; 321: 1306–1311.
Whittaker KW, Ikram K, Anderson DF, Kiel AW, Luff JL . Non-communication between ophthalmologists and optometrists. J Roy Soc Med 1999; 92: 247–248.
Ingram D, Culham L . Ophthalmologists and optometrists—interesting times?. Br J Opthalmol 2001; 85: 769–770.
Burns J, Barrett G, Murdoch IE . The experiences of patients with suspected glaucoma: a qualitative study. Ophthalmic Nurs J 2001; 5(3): 8–11.
Acknowledgements
We thank Helen Baker, Sara Mazhar, Kate Murphy, Jim Kirwan, Dan Rosser, Pak Sang Lee, all the optometrists who participated and our volunteers for their invaluable assistance with this study. This work was supported by the International Glaucoma Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Theodossiades, J., Murdoch, I. & Cousens, S. Glaucoma case finding: a cluster-randomised intervention trial. Eye 18, 483–490 (2004). https://doi.org/10.1038/sj.eye.6700676
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700676
Keywords
This article is cited by
-
Outcomes of newly referred patients with suspected angle closure: do we need to redefine the clinical pathways?
Eye (2024)
-
Referrals from community optometrists to the hospital eye service in Scotland and England
Eye (2022)
-
Evaluation of the effectiveness of ophthalmic assistants as screeners for glaucoma in North India
Eye (2011)
-
Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes
Eye (2010)
-
The influence of the new general ophthalmic services (GOS) contract in optometrist referrals for glaucoma in Scotland
Eye (2009)