Abstract
Purpose
To assess the effect of atypical pattern of retardation (APR) on retinal nerve fibre layer (RNFL) measurements made by scanning laser polarimetry (SLP) with variable corneal compensation (GDx-VCC) in glaucomatous eyes.
Methods
One eye each of 30 glaucomatous patients (average mean deviation (MD): −6.4±4.8) with APR on GDx-VCC retardation map were selected. In total, 34 glaucomatous, age- and severity-matched eyes (average MD: −7.0±5.3) and 36 age-matched healthy subjects, both with a normal pattern of retardation (NPR) represented control groups. APR on retardation maps was characterized by alternating peripapillary circumferential bands of low and high retardation, or high retardation areas arranged in a spokelike pattern, or high retardation nasal and temporal splotchy areas. Typical scan score (TSS) was extracted for each included eye. GDx-VCC parameters (mean±SD) in the two groups of glaucomatous eyes were compared with healthy eyes' corresponding values (Mann–Whitney U-test). Areas under receiver operating characteristic (AUROC) curves were generated to assess the APR effect on the parameters' diagnostic ability.
Results
All parameters discriminated adequately between healthy and glaucomatous eyes with NPR (AUROCs ≥0.9 for nine parameters). On the contrary, considering healthy and glaucomatous eyes with APR, four thickness parameters could not separate the two groups and AUROCs ≥0.85 appeared only for Inferior and Superior Ratio, NFI, Max Modulation.
Conclusion
APR may void the effect of custom compensation and provide spurious RNFL thickness measurements. When a printout of glaucomatous eyes with APR is evaluated, it is proper to rely on ratios, modulation parameters, and NFI, since the diagnostic ability of thickness parameters is significantly reduced.
Similar content being viewed by others
Introduction
Peripapillary retinal nerve fibre layer (RNFL) thickness may be objectively assessed in vivo by scanning laser polarimetry (SLP). Polarized light crossing tissues with form birefringence properties undergoes retardation linearly related to thickness in a primate model.1 The greater the retardation, the thicker the tissue. During the clinical course of glaucomatous optic neuropathy, standard automated perimetry (SAP) detects a glaucoma-related visual field (VF) defect only after at least a 40% loss of retinal ganglion cells has already occurred.2, 3, 4 Instruments measuring optic disc topography and RNFL thickness may assist clinicians in early diagnosis and follow-up of glaucomatous optic neuropathy. Many reports showed that with respect to SLP with fixed compensation (GDx-FCC), the use of variable compensation (GDx-VCC) improves significantly the structure–function relationship5 and diagnostic ability in glaucomatous eyes.6, 7, 8, 9, 10, 11, 12, 13, 14 Moreover, early RNFL thinning in perimetrically unaffected fellow eyes of patients with unilateral glaucoma was detected.15 However, some eyes had to be discarded from these studies because an atypical pattern of retardation (APR) appeared on the retardation map available in the printout.13, 14 Bagga and Greenfield16 recently described in a great detail polarimetric features in these eyes. On average, APR was found to be associated with artefactual increase in RNFL thickness. The source of such high retardation is still unknown, even if it probably arises from undefined subretinal structures.17 To our knowledge, no detailed description about polarimetric features in these eyes is available. The aim of this study was to evaluate the APR effect on RNFL assessment on GDx-VCC in glaucomatous eyes.
Materials and methods
We reviewed charts in the database of patients that underwent peripapillary RNFL evaluation on GDx-VCC at the Glaucoma Unit of Trieste University Eye Clinic between January and October 2004.
Criteria for inclusion in the study were:
-
peripapillary RNFL thickness evaluation by means of GDx-VCC with image quality score ≥8, as provided by software;
-
an APR on the GDx-VCC printout retardation map;
-
SAP performed at ±1 month from SLP, showing a glaucomatous defect;
-
refractive error within the ±5 spherical dioptres range, with less than ±2 cylinder dioptres.
Exclusion criteria were:
-
best-corrected visual acuity (BCVA) ≤20/40;
-
corneal or lens opacity interfering with clinical, SAP, or SLP examination;
-
significant peripapillary atrophy falling under ellipse measurement, tilted disc, uveitis, significant vitreous floaters, diffuse or localized retinal, or macular disease;
-
inability to perform reliable SAP (fixation losses, false-positive or negative rates >20%) or SLP (poor fixation, inattentive patients).
A sample of glaucomatous eyes with normal pattern of retardation (NPR) was selected, after adequate age- and severity matching with glaucomatous subjects and APR. A third sample of age-matched normal subjects with NPR was selected. Any morphologic hint of APR in healthy eyes was a cause for exclusion from the study. One eye each of enrolled subjects was selected randomly for inclusion, if both met eligibility criteria. Each patient underwent a comprehensive clinical examination. BCVA was measured on a standard ETDRS chart. Anterior segment was evaluated on slit lamp, and gonioscopy and Goldmann applanation tonometry were performed. Optic disc was examined by stereo-biomicroscopy with a +78D lens, after pupil dilation. SAP was performed with the Humphrey Field Analyzer (Humphrey Systems, Dublin, CA), 24-2 program, SITA standard strategy.
Healthy subjects had normal SAP (mean deviation (MD)—and pattern standard deviation (PSD)—within 95% confidence limits, Glaucoma Hemifield Test (GHT)—within normal limits), intraocular pressure <21 mmHg, healthy optic disc appearance with intact neuroretinal rim, no history of ocular disease or family history of glaucoma. Glaucomatous optic neuropathy was defined as cupping, rim notching, or diffuse thinning. On SAP, defects were classified as glaucomatous with either GHT outside normal limits or PSD probability <5%. All glaucomatous patients had at least two previous SAP and reproducible VF defects. Grading scale of VF defect severity according to the Hodapp–Parrish–Anderson classification was used.18
SLP was performed with the commercially available device (GDx-VCC, software 5.3.4; Carl Zeiss, Dublin, CA, USA) using an 8-pixel-wide (approximately 0.4 mm in an emmetropic eye) circular calculation area with an inner diameter of 54 pixels (approximately 2.5 mm in an emmetropic eye) centred on the optic disc. The first reading was obtained to measure and compensate anterior segment birefringence. The second reading provided values of RNFL parameters under the calculation area. On both readings, maximum effort was paid to obtain high-quality scans and all eyes had to pass the four-scan quality checks performed by software (alignment, fixation, refraction, and illumination). The correct positioning of the ellipse on the inner margin of peripapillary scleral ring was checked on all eyes by a trained technician (RM).
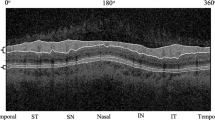
APR was arbitrarily and independently diagnosed by two readers (SDP, OV) in a masked fashion. Agreement rate between readers was 88.2% and only eyes on which readers agreed were included. NPR is characterized by retardation maps with highest retardation superiorly and inferiorly and low retardation nasally and temporally.16 Morphologic diagnosis of APR relied on retardation maps with alternating peripapillary circumferential bands of low and high retardation, or high retardation areas arranged in a spokelike pattern, or high retardation nasal and temporal splotchy areas.16 Then, by exporting each scan raw data on a floppy disk, the typical scan score (TSS) was identified for each included eye. TSS is generated by a support vector machine (SVM)16 and provides values ranging from 0 to 100, so that retardation image atypia increases with decreasing TSS (Figure 1). Cut-off was arbitrarily placed at the value of 70.
A 74-year-old female (left panel) with dense arcuate glaucomatous defect on SAP (MD −9.83 dB, PSD 15.43). On the GDx-VCC retardation map, a marked APR is present. TSS is 24. All parameters are green-flagged (probability ≥5%) and NFI is 31. A 71-year-old male (right panel) with dense superior defect on SAP (MD −11.35 dB, PSD 13.05). A borderline or mild APR is present on the retardation map (TSS=66). NFI is 44.
Parameters considered were ellipse average and standard deviation (TSNIT average and SD), superior and inferior average (SA, IA), nerve fibre indicator (NFI), superior and inferior ratio (SR, IR), superior/nasal ratio (S/N), maximum modulation (MM), superior and inferior maximum (SM, IM), ellipse modulation (EM), normalized superior and inferior area (NSA, NIA).
Mean values (±SD) for age, MD, PSD and TSS in the three groups were compared on ANOVA. When overall ANOVA was statistically significant (P<0.05), pairwise comparisons were performed by the Tukey HSD test. Mean values (±SD) of each parameter were compared by the Mann–Whitney U-test in healthy eyes and the two groups of glaucomatous eyes. For each parameter, areas under receiver operating characteristic (AUROC) curves were generated to assess their diagnostic ability, separately for the two groups of glaucomatous eyes. Differences in their values were evaluated with the DeLong method.19 Statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Each patient was fully aware about the aim of the study and signed informed consent. Methods were approved by the internal Ethics Committee and adhered to the tenets of the Helsinki Declaration for research involving human subjects.
Results
On the basis of SAP, morphologic analysis of GDx-VCC printout and TSS value, 30 subjects were enrolled in the glaucoma with APR group. Control groups comprised 34 glaucomatous, age- and severity-matched patients with an NPR and 36 healthy subjects with NPR. Demographics, mean SAP indexes, and TSS of the three groups are shown in Table 1. On ANOVA, P was <0.001 for MD, PSD, and TSS. VF defect severity grading scale was similar in the two groups of glaucomatous eyes (P=0.65 on χ2 test). In Table 2, mean values (±SD) for each parameter are shown separately for healthy and for the two groups of glaucomatous eyes. All parameters resulted significantly different between healthy eyes and glaucomatous eyes with NPR. When healthy and glaucomatous eyes with APR were compared, only NFI, TSNIT SD, NSA, ratio, and modulation parameters resulted significantly different (P<0.001), whereas TSNIT Average, SM, IA, and IM could not separate the two groups. In Table 3, AUROCs evaluating discrimination between healthy and glaucomatous eyes with NPR and APR are presented. Best-performing parameters in separating healthy from glaucomatous eyes with NPR were NFI, all thickness parameters and normalized areas (all with AUROC>0.9). On the contrary, when discriminating between healthy and glaucomatous eyes with APR, best-performing parameters were IR and SR, followed by NFI, TSNIT SD, and modulation parameters (AUROCs range: 0.89–0.81), whereas thickness parameters performed much worse. Differences for areas (Table 3) showed that, with respect to NPR, the presence of APR is associated with significant decrease of their values for thickness parameters (Figure 2, left), significant increase for IR (Figure 2, right), SR and MM, and minimal, not significant, variation for TSNIT SD, S/N, NFI, and EM.
Discussion
In previous studies on GDx-FCC, ratios and parameters describing relative thickness often performed better than those purely quantifying RNFL thickness when diagnostic ability for glaucoma was evaluated.20, 21 Residual anterior segment birefringence, not compensated by FCC, was considered to be the cause.22
We found similarities between those reports and our glaucomatous eyes with APR, in spite of GDx-VCC use. In these eyes, customized compensation is only partially effective, meaning that APR is somewhat independent of GDx-VCC use. Recently, both for healthy and glaucomatous eyes, a strong correlation between APR and falsely increased thickness in mean, inferior, temporal, and nasal RNFL was demonstrated.16 The nature of APR remains unexplained, even if the presence of another source of diffuse retardation, due to structures with birefringent properties other than RNFL, has been postulated.17
We found that APR may significantly interfere with RNFL measurements in glaucomatous eyes, in spite of GDx-VCC use. Differently from what is observed for glaucomatous eyes with NPR, parameters such as TSNIT Average, IA, SM, and IM did not separate healthy eyes from glaucomatous eyes with APR (Table 2), and their AUROCs (Table 3) indicated a poor discriminating ability (areas never larger than 0.6), with IM showing a chance discrimination (area=0.49). On the contrary, NFI and parameters independent of absolute RNFL thickness (ratios, modulations, TSNIT SD) showed a good diagnostic ability in this peculiar group of eyes (Tables 2 and 3), testifying no or minimal influence by APR.
Prior to performing this study, there was clinical suspicion that glaucomatous eyes with NPR and those with APR fared quite differently in terms of RNFL measurements with respect to healthy eyes. In order to confirm this suspicion, both groups were compared with a single group of healthy eyes, including only eyes with an NPR. Glaucomatous eyes with NPR and APR were intentionally matched for age and disease severity (Table 1) and then GDx-VCC parameters should have disclosed similar AUROCs in the two groups. However, it may be noted that APR presence was associated with significant variations in area values (Table 3, Figure 2). An overall, apparent heightening of the whole 360° TSNIT thickness profile may be hypothesized, that probably affected the diagnostic performance of thickness parameters. These findings advise to using different methods to evaluate summary data in glaucomatous eyes with APR.
This study has two potential flaws. The first is that the presence of APR was determined by means of morphological analysis of the retardation map. Only after that was TSS extracted for each included eye. Anyway, a similar procedure was previously used.16 By considering TSS values in the three groups (Table 1), it may be noted that morphologic selection was accurate enough. No standardized TSS cut-off value is currently available, so in order to separate eyes with NPR from those with APR, we arbitrarily chose a cut-off of 70. The second one is the relatively small sample of glaucomatous eyes with APR included. This means that further studies are necessary to reach a better definition of polarimetric features in these eyes.
It remains to identify the appropriate procedure to evaluate the GDx-VCC printout in glaucomatous eyes with APR. In previous studies, these eyes were excluded from calculations, since some of them were deemed by software not to be compatible with a normative database.13, 14 In clinical studies they may be excluded, even if for future research the exclusion of eyes with TSS ≤60 has been proposed,16 but for daily clinical practice, our results suggest that they may nevertheless be evaluated by GDx-VCC, relying on NFI, TSNIT SD, ratio, and modulation parameters, not on thickness parameters.
References
Weinreb RN, Dreher AW, Coleman A, Quigley H, Shaw B, Reiter K . Histopathologic validation of Fourier-ellipsometry measurements of retinal nerve fiber layer thickness. Arch Ophthalmol 1990; 108: 557–560.
Pederson JE, Anderson DR . The mode of progressive optic disc cupping in ocular hypertension and glaucoma. Arch Ophthalmol 1980; 98: 490–495.
Quigley HA, Addicks EM, Green RW . Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol 1982; 100: 135–146.
Sommer A, Katz J, Quigley HA, Miller NR, Robin AL, Richter RC et al. Clinically detectable nerve fiber layer atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol 1991; 109: 77–83.
Reus NJ, Colen TP, Lemij HG . Visualization of localized retinal nerve fiber layer defects with the GDx with individualized and with fixed compensation of anterior segment birefringence. Ophthalmology 2003; 110: 1512–1516.
Weinreb RN, Bowd C, Zangwill LM . Glaucoma detection using scanning laser polarimetry with variable corneal polarization compensation. Arch Ophthalmol 2002; 120: 218–224.
Choplin NT, Zhou Q, Knighton RW . Effect of individualized compensation for anterior segment birefringence on retinal nerve fiber layer assessment as determined by scanning laser polarimetry. Ophthalmology 2003; 110: 719–725.
Bowd C, Zangwill LM, Weinreb RN . Association between scanning laser laser polarimetry measurements using variable corneal polarization compensation and visual field sensitivity in glaucomatous eyes. Arch Ophthalmol 2003; 121: 961–966.
Medeiros FA, Zangwill LM, Bowd C, Bernd AS, Weinreb RN . Fourier analysis of scanning laser polarimetry measurements with variable corneal compensation in glaucoma. Invest Ophthalmol Vis Sci 2003; 44: 2606–2612.
Reus NJ, Lemij HG . The relationship between standard automated perimetry and GDx VCC measurements. Invest Ophthalmol Vis Sci 2004; 45: 840–845.
Schlottmann PG, De Cilla S, Greenfield DS, Caprioli J, Garway-Heath DF . Relationship between visual field sensitivity and retinal nerve fiber layer thickness as measured by scanning laser polarimetry. Invest Ophthalmol Vis Sci 2004; 45: 1823–1829.
Tannenbaum D, Hoffmann D, Lemij HG, Garway-Heath DF, Greenfield DS, Caprioli J . Variable corneal compensation improves the discrimination between normal and glaucomatous eyes with the scanning laser polarimeter. Ophthalmology 2004; 111: 259–264.
Reus NJ, Lemij HG . Diagnostic accuracy of the GDx VCC for glaucoma. Ophthalmology 2004; 111: 1860–1865.
Medeiros FA, Zangwill LM, Bowd C, Weinreb RN . Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomography for the detection of glaucoma. Arch Ophthalmol 2004; 122: 827–837.
Reus NJ, Lemij HG . Scanning laser polarimetry of the retinal nerve fiber layer in perimetrically unaffected eyes of glaucoma patients. Ophthalmology 2004; 111: 2199–2203.
Bagga H, Greenfield DS . Quantitative assessment of atypical birefringence images using scanning laser polarimetry with variable corneal compensation. Am J Ophthalmol 2005; 139: 437–446.
Burns SA, Elsner AE, Mellem-Kairala MB, Simmons RB . Improved contrast of subretinal structures using polarization analysis. Invest Ophthalmol Vis Sci 2003; 44: 4061–4068.
Hodapp E, Parrish II RK, Anderson DR . Clinical Decisions in Glaucoma. Mosby-Year Book: St Louis, 1993, pp 52–61.
DeLong ER, DeLong DM, Clarke-Pearson D . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Bowd C, Zangwill LM, Berry CC, Blumenthal EZ, Vasile C, Sanchez-Galeana C et al. Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Invest Ophthalmol Vis Sci 2001; 42: 1993–2003.
Zangwill LM, Bowd C, Berry CC, Williams J, Blumenthal EZ, Sanchez-Galeana CA et al. Discriminating between normal and glaucomatous eyes using the Heidelberg retina tomograph, GDx nerve fiber analyzer, and optical coherence tomography. Arch Ophthalmol 2001; 119: 985–993.
Greenfield DS, Knighton RW, Feuer WJ, Schiffman JC, Zangwill LM, Weinreb RN . Correction for corneal polarization axis improves the discriminating power of scanning laser polarimetry. Am J Ophthalmol 2002; 134: 27–33.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors have any financial or proprietary interest with products cited in the text
Rights and permissions
About this article
Cite this article
Da Pozzo, S., Marchesan, R., Canziani, T. et al. Atypical pattern of retardation on GDx-VCC and its effect on retinal nerve fibre layer evaluation in glaucomatous eyes. Eye 20, 769–775 (2006). https://doi.org/10.1038/sj.eye.6701997
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701997
Keywords
This article is cited by
-
The glaucoma detection capability of spectral-domain OCT and GDx-VCC deviation maps in early glaucoma patients with localized visual field defects
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)
-
Test–retest variability in structural parameters measured with glaucoma imaging devices
Japanese Journal of Ophthalmology (2013)
-
Clinical characteristics of eyes demonstrating atypical patterns in scanning laser polarimetry
Eye (2008)
-
Correlation between optic disc area and retinal nerve fiber layer thickness: a study on scanning laser polarimetry with variable corneal compensation
Graefe's Archive for Clinical and Experimental Ophthalmology (2007)
-
Effect of posterior capsular opacification removal on scanning laser polarimetry measurements
Graefe's Archive for Clinical and Experimental Ophthalmology (2006)