Abstract
Aim
To determine the prevalence of glaucoma in patients with obstructive sleep apnoea.
Design
Cross-sectional case series.
Participants
One hundred patients with moderate to severe obstructive sleep apnoea.
Testing
Within 48 h of the polysomnographic diagnosis of obstructive sleep apnoea, patients underwent the following tests: intraocular pressure, gonioscopy, automated perimetry, stereoscopic biomicroscopy, and fundascopic assessment for the presence of glaucomatous optic nerve changes.
Main outcome measures
The prevalence of glaucoma in patients with obstructive sleep apnoea and the associations between patient characteristics and both glaucoma and intraocular pressure.
Results
Glaucoma was diagnosed in 27 of 100 patients yielding an estimated prevalence of 27% (95% CI 19–37%). The presence of glaucoma did not correlate with sex, body mass index (BMI), or AHI, but did appear to be associated with age (P=0.014). There was no evidence of a relationship between intraocular pressure and either the apnoea plus hypopnoea index or age.
Conclusion
The prevalence of glaucoma in patients with obstructive sleep apnoea is an estimated 27%. Sex, age, body mass index or apnoea plus hypopnoea index are not factors influencing the presence of glaucoma in this population of patients.
Similar content being viewed by others
Introduction
Glaucoma affects an estimated 3 million Americans, with resultant blindness in 120 000. Loss of integrity of the optic nerve is key in the pathogenesis of this condition. Several reports suggest the importance of vascular risk factors, especially in normal tension glaucoma.1, 2, 3 Obstructive sleep apnoea (OSA) is a condition characterized by recurrent upper airway obstruction accompanied by hypoxemia, hypercapnia, and sleep disruption. Untreated OSA has been implicated in the development of cerebral ischaemia, myocardial infarction, pulmonary hypertension, and cardiac rhythm disturbances, all potential factors in optic nerve ischaemia.
It has been suggested that patients with OSA are at significant risk of developing primary open-angle glaucoma (POAG) and normal tension glaucoma (NTG).4, 5, 6, 7, 8, 9, 10, 11 Kargi et al5 found diffusely decreased retinal nerve fibre layer thickness (RNFL) (an early finding in glaucoma) in patients with sleep apnoea compared with controls and the severity of OSA, as judged by the apnoea–hypopnoea index, was strongly correlated with the decrease in RNFL. Using standard diagnostic techniques for glaucoma, Mojon et al6 reported a case series of 114 patients referred for polysomnography (PSG) for the evaluation of OSA. Sixty-nine patients had OSA confirmed by PSG, and 5 (7.2%) of these patients were diagnosed with glaucoma.
Two studies have found no association of OSA with glaucoma. Geyer et al12 examined 228 patients diagnosed with OSA from a single sleep centre and found the prevalence of glaucoma to be 2%, the same as expected in a general Caucasian population. Girkin et al13 looked for associated diagnoses of sleep apnoea in 667 newly diagnosed glaucoma patients in a single institution's database and compared the association with a control group and did not find it to be significantly different, although a trend of more prevalent glaucoma diagnosis in patients with OSA was noted.
The true prevalence of glaucoma in sleep apnoea is not clear from the literature available. If the association is indeed present, treatment of obstructive sleep apnoea may represent a modifiable risk factor in the development and progression of glaucoma. We report our review of the prevalence of glaucoma in a population of patients with moderate to severe OSA.
Patients and methods
The Institutional Review Board of the Mayo Clinic approved the experimental protocol. Subjects were selected from patients who were referred for sleep medicine evaluation for possible OSA. After sleep medicine evaluation, all patients suspected of having OSA who met accepted clinical criteria (eg daytime hypersomnolence, snoring, and witnessed apnoea) underwent standard overnight PSG. Those confirmed to have OSA (apnoea plus hypopnoea index (AHI) >15) were eligible for the study. Patients with obstructive sleep apnoea, who had a previous established diagnosis of glaucoma, and/or who were already on treatment for glaucoma were noted and included in the prevalence calculation. Only patients who could undergo an overnight PSG and ophthalmologic examination were included. In this case series, 117 consecutive patients with confirmed OSA were recruited for the study. Patients 17/117 refused to undergo an eye exam and were not eligible to be included in the study. Those eligible underwent a complete ophthalmologic examination within 48 h of the PSG. All ophthalmic examinations were performed by a single glaucoma specialist and included measurement of intraocular pressure (IOP), gonioscopy, automated perimetry, stereoscopic biomicroscopy, and fundoscopic assessment for the presence of glaucomatous optic disc changes. The diagnostic criteria used by the examiner were strict adherence to the latest Primary Open Angle Glaucoma Preferred Practice Pattern's definition and diagnostic recommendations.14 The definition of glaucoma is a multifactorial optic neuropathy in which there is a characteristic acquired loss of retinal ganglion cells and atrophy of the optic nerve and/or characteristic visual field defects. The presence of the following in the optic disc or retinal nerve fibre layer diffuse or focal narrowing or notching of the disc rim, especially at the inferior or superior poles; diffuse or localized abnormalities of the retinal nerve fibre layer, especially at the inferior or superior poles; nerve fibre layer haemorrhages; asymmetrical appearance of the optic disc rim between fellow eyes that suggests loss of neural tissue. All optic nerves that were diagnosed as glaucomatous had a cup/disc ratio (c/d) of greater than 0.7, peripapillary retinal pigment epithelial atrophy, asymmetry of c/d ratio greater than 0.2 between the two eyes and/or more than 2 h of optic nerve rim thinning consistent with glaucoma. Visual fields were defined as glaucomatous by following these selected guidelines that were taken from the modified Collaborative Initial Glaucoma Treatment Study guidelines.15 Visual field defects included the presence of one or more of the following abnormalities in the visual field in the absence of other explanations for a field defect in the following locations with a cluster of three adjacent depressed points on the pattern standard deviation plot a nasal step or scotoma, inferior or superior arcuate scotoma, paracentral scotoma, or generalized depression. Additional criteria were abnormal glaucoma hemifield tests and/or a mean deviation >5. The defects and/or visual field parameters were persistent on at least two visual field tests using the 24-2 SITA Standard Humphrey automated threshold perimeter. At the time of the ophthalmologic examination, the results of the polysomnogram (degree of sleep apnoea) were unknown to the examiner.
Numerical data was summarized with the sample median and range. The prevalence of glaucoma in OSA patients were estimated along with an exact binomial 95% confidence interval (CI). Fisher's exact test, Wilcoxon's rank sum test, and Kendall's were used to investigate possible associations between patient characteristics and both glaucoma and IOP.
Results
Patient characteristics are shown in Table 1. Glaucoma was diagnosed in 27 of 100 patients yielding an estimated prevalence of 27% (95% CI19–37%). The diagnosis was established by visual field and nerve appearance in 14% (findings noted in one eye in 4 patients and both eyes in 10 patients), by nerve only in 9% (findings noted in one eye in 5 patients and both eyes in 4 patients) and by history and outside record review of pre-existing glaucoma which was under treatment by an outside ophthalmologist in 4% Table 2. The presence of glaucoma did not correlate with sex, body mass index (BMI), or AHI, but appeared to be associated with age (P=0.014). The median age of glaucoma patients was 67 compared with 59 for patients without glaucoma. An elevated IOP in at least one eye without other evidence of glaucoma was present in 6%. In these patients with ocular hypertension, the IOP ranged between 18 and 28 with a median of 22. In review of all patients, there was overall evidence that IOP increases as BMI increases (P=0.006) and that IOP was lower in men than in woman (P=0.015). Median IOP for women was 17.0 and 15.3 for men. There was no evidence of a relationship between IOP and either AHI or age.
Discussion
Our study revealed an unexpectedly high rate of glaucoma in patients with obstructive sleep apnoea. Our findings are consistent with the higher than expected rate of glaucoma reported by other authors.4, 5, 6, 7, 8, 9, 10, 11 We recognize that the study design has the potential to introduce bias since the eye examinations were carried out with the knowledge that all the patients had obstructive sleep apnoea. The use of strict optic nerve and visual field criteria for glaucoma diagnosis was employed in an attempt to overcome this bias.
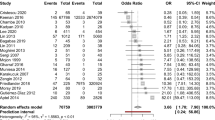
Most of the studies in the literature show a greater prevalence of glaucoma in patients with OSA or a greater than expected prevalence of OSA in patients with glaucoma than is found in a matched control group or historical controls. Mojon et al9 have carried out a series of studies examining the prevalence of glaucoma in patients with OSA and the prevalence of OSA in glaucoma patients. They were the first to show an increased prevalence of glaucoma in a population with newly diagnosed OSA of 7.2%. If we used the same diagnostic criteria for glaucoma that Mojon did, our prevalence would be 18%. The change stems from a re-categorization of our 9% diagnosed by optic nerve changes only as glaucoma suspects rather than glaucoma, which is currently preperimetric.
Our study is consistent with the studies referenced above for an association of OSA and glaucoma. In our study, the patients with glaucoma did not have elevated IOP, a major risk factor for glaucoma. These patients have glaucoma as defined earlier, which is multifactorial (IOP is a risk factor), with the possibility that their OSA was a factor in the development of their glaucoma. Six percent of the OSA subject were diagnosed as ocular hypertensives with only an elevated IOP and no signs of glaucoma.
The lack of a correlation between AHI and the presence of glaucoma in the study reported here was surprising in view of the higher than expected prevalence of glaucoma in our population of patients with moderately severe obstructive sleep apnoea. Others have found a correlation.6, 16 Factors that affect oxygenation of the optic nerve, which we did not measure, may have played a role. These include blood pressure, cardiac output, and neurohormone levels. The measurement of AHI has become the standard for statistical review in studies of sleep apnoea patients, but it is far from being the only measure of the effect of disordered breathing on haemodynamics, metabolic function, and daytime symptoms. In addition, in any given patient, the AHI does not always reflect the degree of hypoxaemia or the haemodynamic derangements, which are also influenced by the baseline respiratory status, baseline cardiac output, and the length of individual apnoeas and hypopnoeas. Non-apneic snoring has been independently associated with hypertension, suggesting that patients with obstructive sleep apnoea and AHI levels much lower than those in our study have significant changes in haemodynamics.17
Two studies in the literature have not shown sleep apnoea to be a risk factor for glaucoma. The first was published by Geyer et al12 and found a prevalence of glaucoma of only 2% among 228 patients with sleep apnoea, not significantly different from that of the general Caucasian population. In that study, patients previously studied and found to have sleep apnoea were recalled to participate in the study. The time lapse between the sleep study and the eye examination was not noted by the authors. It is likely that most of those who participated in the study were receiving some form of therapy for OSA with the majority receiving nasal continuous positive airway pressure (nCPAP). Two recent reports suggest that treatment of OSA may halt the progression of glaucoma.18, 19 It is conceivable that the rate of glaucoma would have been higher in the study by Geyer et al if the eye examination had taken place before the institution of treatment for OSA. Alternatively, the difference between our report and the one by Geyer et al might be due to differences in age, OSA severity, and BMI noted between their population of patients and ours. Comparing the data, our subjects were older, more obese, and had more severe OSA. The median AHI in our patients was 37, indicating that our group as a whole had moderately severe OSA. This is a group that would be expected to have more profound changes in oxygenation and circulatory haemodynamics, as Kargi et al5 have shown, where the apnoea–hypopnea index strongly correlates with the decrease in RNFL. Finally, the study reported by Geyer et al showed a prevalence of pre-existing glaucoma of only 0.4% compared with 4% in our population of patients, suggesting that the populations studied might have had significant differences in the prevalence of glaucoma. The second study by Girkin et al13 examined three International Classification of Diseases Ninth Revision (ICD9) diagnostic codes for newly diagnosed glaucoma over a 4-year time frame and also searched for sleep apnoea diagnoses under a single diagnostic ICD9 code. They found 667 patients with newly diagnosed glaucoma, and a control group without glaucoma of 10 matched controls for each case of glaucoma were found from the diagnostic data base. The investigators acknowledge that this methodology favours the null outcome of an association between glaucoma and sleep apnoea. Additionally, a review of ICD9 codes reveals that at least nine other additional codes for sleep apnoea are available, which were not considered by these investigators, as they searched for only one ICD9 diagnostic code, leaving a potential for patients diagnosed with another sleep apnoea code not to be detected. Additionally, the investigators have no way of determining which patients may have been obtaining eye care or care of their OSA outside of the institution, in which case an unknown quantity of diagnoses would not be in their database. The inherent methodologic differences and weaknesses of this study make it difficult to compare with our results.
Mojon has reported two additional studies examining the prevalence of newly diagnosed sleep apnoea in patients with POAG (20% vs 11%) and NTG (44 vs 3.3%) and found that the prevalence of OSA was significantly higher in the glaucoma patients compared with the control groups.8, 9 Marcus et al10 performed a very similar study where they examined the prevalence of OSA in patients who were NTG suspects or NTG patients and compared it with a matched control group. OSA was found to be present in 3% of the control group compared with 43% of the NTG suspects and 57% of the patients with NTG. The patients in the Marcus study were initially diagnosed by history and most were confirmed by polysomnography. A fourth study by Onen et al11 also found a significantly higher prevalence of patients with sleep-disorded breathing who were diagnosed with glaucoma as compared with a matched group of patients in their practice without glaucoma. None of the patients had a confirmed OSA diagnosis by polysomnography and were historical diagnoses only.
The finding of a higher than expected prevalence of glaucoma in our patient population with sleep apnoea suggests that clinicians may need to consider the possibility that unrecognized glaucoma is present in patients with newly diagnosed or existing sleep apnoea. Our study did not address the issue of prevalence of sleep apnoea in patients with glaucoma and further studies will be needed to determine if glaucoma patients have a higher than expected rate of obstructive sleep apnoea.
References
Drance SM . Some factors in the production of low tension glaucoma. Br J Ophthalmol 1972; 56: 229–242.
Flammer J . The vascular concept of glaucoma. Surv Ophthalmol 1994; 38: 3–6.
Kremmer S, Selbach JM, Schäfers R, Philipp T, Steuhl KP. Das kardiovaskuläre Risikoprofil bei der Progression der Glaukomerkrankung. Dt Ärzteblatt 2000; 34/35: 2241–2245.
Walsh JT, Montplasir J . Familial glaucoma with sleep apnoea: a new syndrome? Thorax 1982; 37: 845–849.
Kargi SH, Altin R, Koksa M, Kart L, Cinar F, Ugurbar SH et al. Retinal nerve fibre layer measurements are reduced in patients with obstructive sleep apnoea syndrome. Eye 2005; 19 (5): 575–579.
Mojon DS, Hess CW, Goldblum D, Fleischhauer J, Korner F, Bassetti C et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology 1999; 106: 1009–1012.
Tsang CS, Chong SL, Ho CK, Li MF . Moderate to severe obstructive sleep apnoea patients is associated with a higher incidence of visual field defect. Eye 2006; 20 (1): 38–42.
Mojon DS, Hess CW, Goldblum D, Bohnke M, Korner F, Mathis J . Primary open-angle glaucoma is associated with sleep apnea syndrome. Ophthalmologica 2000; 214: 115–118.
Mojon DS, Hess CW, Goldblum D, Bohnke M, Korner F, Gugger M et al. Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica 2002; 216: 180–184.
Marcus DM, Costarides AP, Gokhale P, Papastergiou G, Miller JJ, Johnson MH et al. Sleep disorders: a risk factor for normal-tension glaucoma? J Glaucoma 2001; 10 (3): 177–183.
Onen SH, Mouriaux F, Berramdane L, Dascotte JC, Kulik JF, Rouland JF . High prevalence of sleep-disordered breathing in patients with primary open-angle glaucoma. Acta Ophthalmol Scand 2000; 78 (6): 638–641.
Geyer O, Cohen N, Segev E, Rath EZ, Melamud L, Peled R et al. The prevalence of glaucoma in patients with sleep apnea syndrome: same as in the general population. Am J Ophthalmol 2003; 136: 1093–1096.
Girkin CA, McGwin Jr G, McNeal SF, Owsley C . Is there an association between pre-existing sleep apnoea and the development of glaucoma? Br J Ophthalmol 2006; 90 (6): 679–681.
American Academy of Ophthalmology. Primary Open-Angle Glaucoma, Preferred Practice Pattern. American Academy of Ophthalmology: San Francisco, 2003. www.aao.org/ppp.
Gillespie BW, Musch DC, Guier KE, Mills RP, Lichter PR, CIGTS Study Group et al. The collaborative initial glaucoma treatment study: baseline visual field and test-retest variability. Invest Ophthalmol Vis Sci 2003; 44 (6): 2613–2620.
Sergi M, Salerno DE, Rizzi M, Blini M, Andreoli A, Messenio D et al. Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma 2007; 16 (1): 42–46.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Leiby BE, Vela-Bueno A et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160: 2289–2295.
Kremmer S, Niederdraing N, Ayertey HD, Steuhl KP, Selbach JM . Obstructive sleep apnea syndrome, normal tension glaucoma, and nCPAP therapy—a short note. Sleep 2003; 26: 161–162.
Sebastian RT, Johns S, Gibson RA . Treating obstructive sleep apnoea syndrome: does it improve visual field changes? Eye 2006; 20 (1): 118–120.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bendel, R., Kaplan, J., Heckman, M. et al. Prevalence of glaucoma in patients with obstructive sleep apnoea—a cross-sectional case-series. Eye 22, 1105–1109 (2008). https://doi.org/10.1038/sj.eye.6702846
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702846
Keywords
This article is cited by
-
The effect of positive airway pressure therapy on intraocular pressure and retina in severe obstructive apnea syndrome
Sleep and Biological Rhythms (2022)
-
Ganglion cell layer thickening in patients suffering from Obstructive Sleep Apnea–Hypopnea syndrome with long Mean Apnea–Hypopnea Duration during sleep
International Ophthalmology (2021)
-
Thinning of the inner and outer retinal layers, including the ganglion cell layer and photoreceptor layers, in obstructive sleep apnea and hypopnea syndrome unrelated to the disease severity
International Ophthalmology (2021)
-
The Associations of Obstructive Sleep Apnea and Eye Disorders: Potential Insights into Pathogenesis and Treatment
Current Sleep Medicine Reports (2021)
-
Visual field defects and retinal nerve fiber imaging in patients with obstructive sleep apnea syndrome and in healthy controls
BMC Ophthalmology (2018)